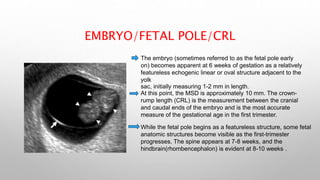
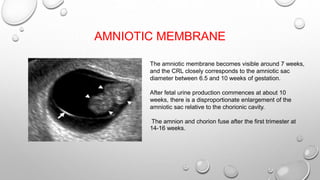
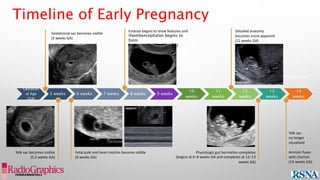
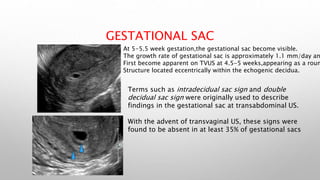
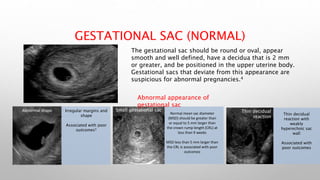
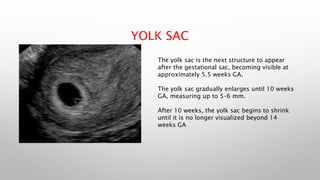
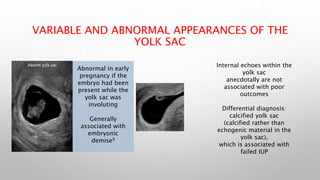
The document provides information on normal sonological findings in the first trimester of pregnancy. It discusses the visualization of structures like the gestational sac, yolk sac, fetal pole, amniotic membrane, and fetal heart during transvaginal ultrasounds between 5-13 weeks of gestation. Key milestones include the gestational sac being visible at 5 weeks, yolk sac at 5.5 weeks, fetal pole and heart at 6 weeks, and detailed anatomy becoming apparent by 12 weeks. Abnormal appearances that could indicate problems are also described.


![ASSESSMENT OF GA
• DETERMINATION OF GA IS MORE ACCURATE THE EARLIER US IS PERFORMED.
• MSD MEASUREMENTS ARE NOT RECOMMENDED FOR ESTIMATING DUE DATE.
• CRL IS THE MOST ACCURATE METHOD TO ESTABLISH GA (UP TO AND INCLUDING 13 6/7
WEEKS OF GESTATION).
• BEYOND A CRL OF 84 MM (14 WEEKS, 0 DAYS), DATING ON THE BASIS OF CRL BECOMES LESS
ACCURATE, AND OTHER SECOND-TRIMESTER BIOMETRIC PARAMETERS SHOULD BE USED.
THESE PARAMETERS (BIPARIETAL DIAMETER, ABDOMINAL CIRCUMFERENCE, HEAD
CIRCUMFERENCE, AND FEMUR LENGTH) ARE USED TO DETERMINE THE ARITHMETIC US AGE.
• AT A GA OF 8 6/7 WEEKS OR LESS (BASED ON LAST MENSTRUAL PERIOD [LMP]), US DATING
SHOULD BE USED IF THE LMP DATING AND US DATING DIFFER BY MORE THAN 5 DAYS.
• AT A GA BETWEEN 9 0/7 WEEKS AND 13 6/7 WEEKS (ON THE BASIS OF THE LMP), US DATING
SHOULD BE USED IF THE LMP DATING AND US DATING DIFFER BY MORE THAN 7 DAYS.
• THE ESTIMATED DUE DATE (EDD), IF BASED ON US DATING, SHOULD BE BASED ON THE
EARLIEST US EXAMINATION OF A CRL MEASUREMENT. CHANGES TO THE EDD SHOULD BE
RESERVED FOR RARE CIRCUMSTANCES.](https://image.slidesharecdn.com/normalsonologicalfindinginfristtrimester-240416200319-fd2c0d98/85/NORMAL-SONOLOGICAL-FINDING-IN-FRIST-TRIMESTER-pptx-17-320.jpg)