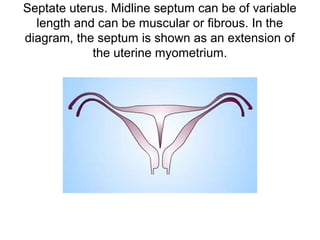
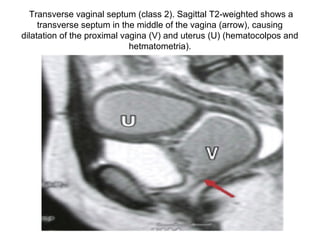
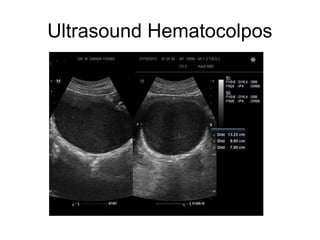
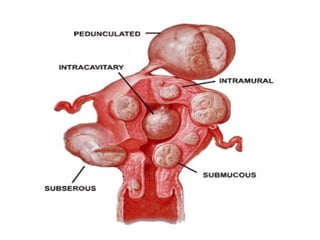
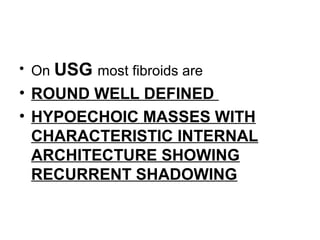
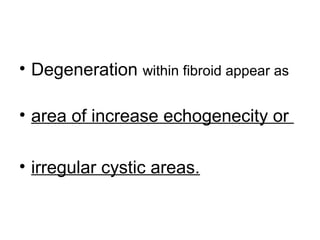
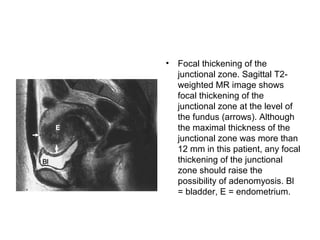
The document provides an overview of the normal radiological anatomy of the female pelvic organs including the uterus, endometrium, myometrium, cervix, vagina, ovaries and their appearance on ultrasound and MRI. It then discusses common uterine abnormalities such as congenital uterine anomalies, fibroids, adenomyosis and their imaging features. In adenomyosis, endometrial glands are present within the myometrium which can appear heterogeneous on ultrasound and cause diffuse or focal thickening of the junctional zone on MRI. Uterine fibroids appear as well-defined hypoechoic masses on ultrasound and may cause various signal changes on MRI depending on factors like degeneration. Congenital anomalies result from






























































































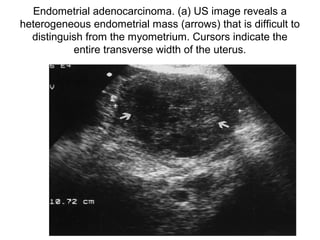





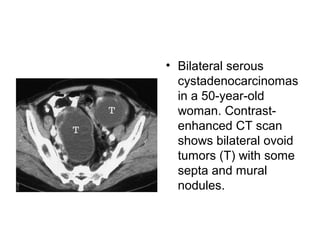
![• Endometrial
carcinoma in a 58-
year-old patient. (a)
Sagittal fast SE T2-
weighted (4,000/119
[effective]) MR image
shows nodular,
discretely irregular
foci of low signal
intensity (arrowheads)
in the endometrial
cavity.](https://image.slidesharecdn.com/gynaecologicalimaging5-160613023211/85/Gynaecological-imaging-116-320.jpg)















































![• Ovarian fibromas are composed of
spindle cells that form collagen and
usually display low signal intensity
on both T1- and T2-weighted MRI.
High signal intensity on T2-
weighted images corresponded to
regions of hyalinization and
myxomatous changes [5].
Intratumoral edema is also
common in larger fibromas.](https://image.slidesharecdn.com/gynaecologicalimaging5-160613023211/85/Gynaecological-imaging-171-320.jpg)