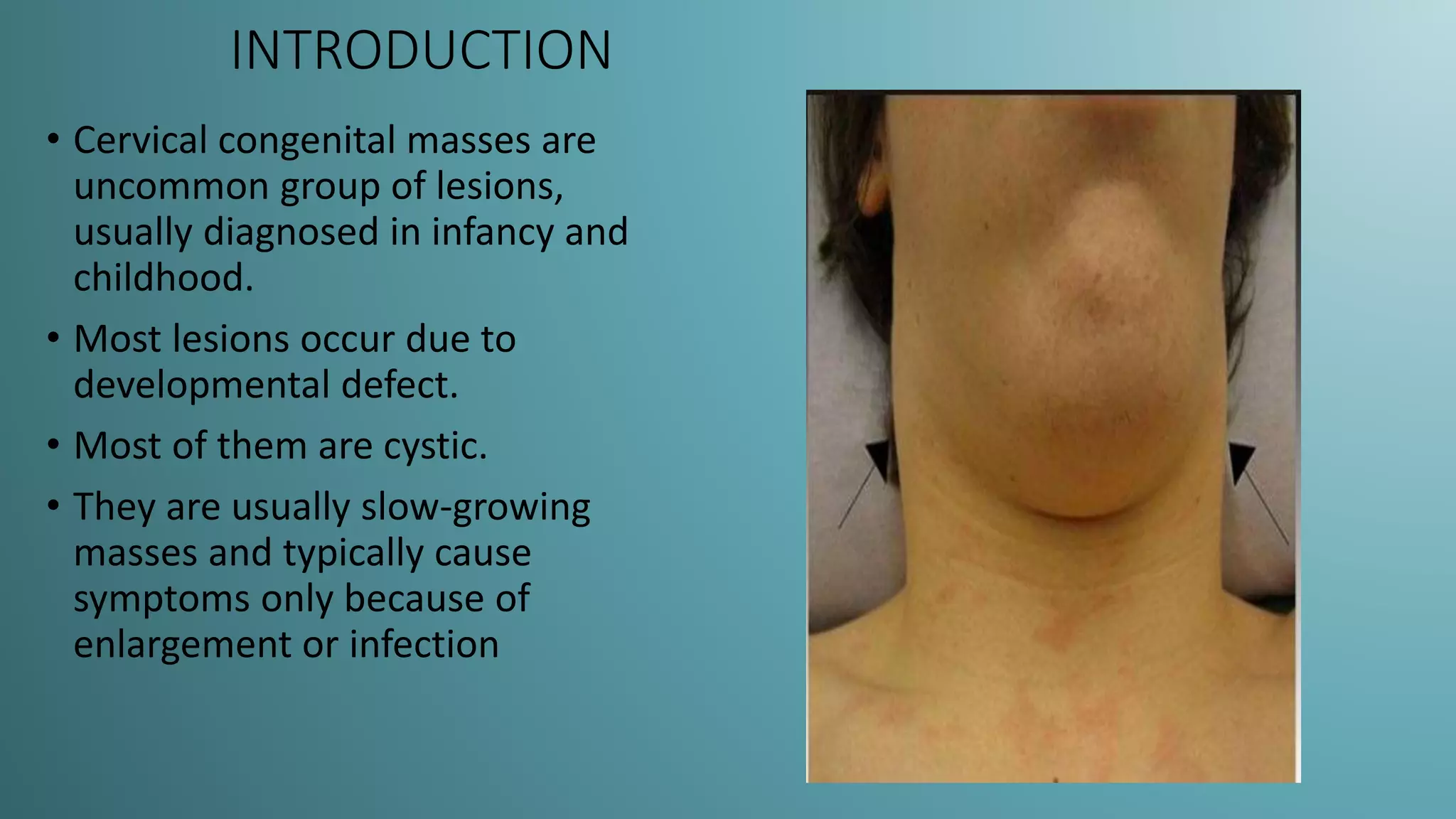
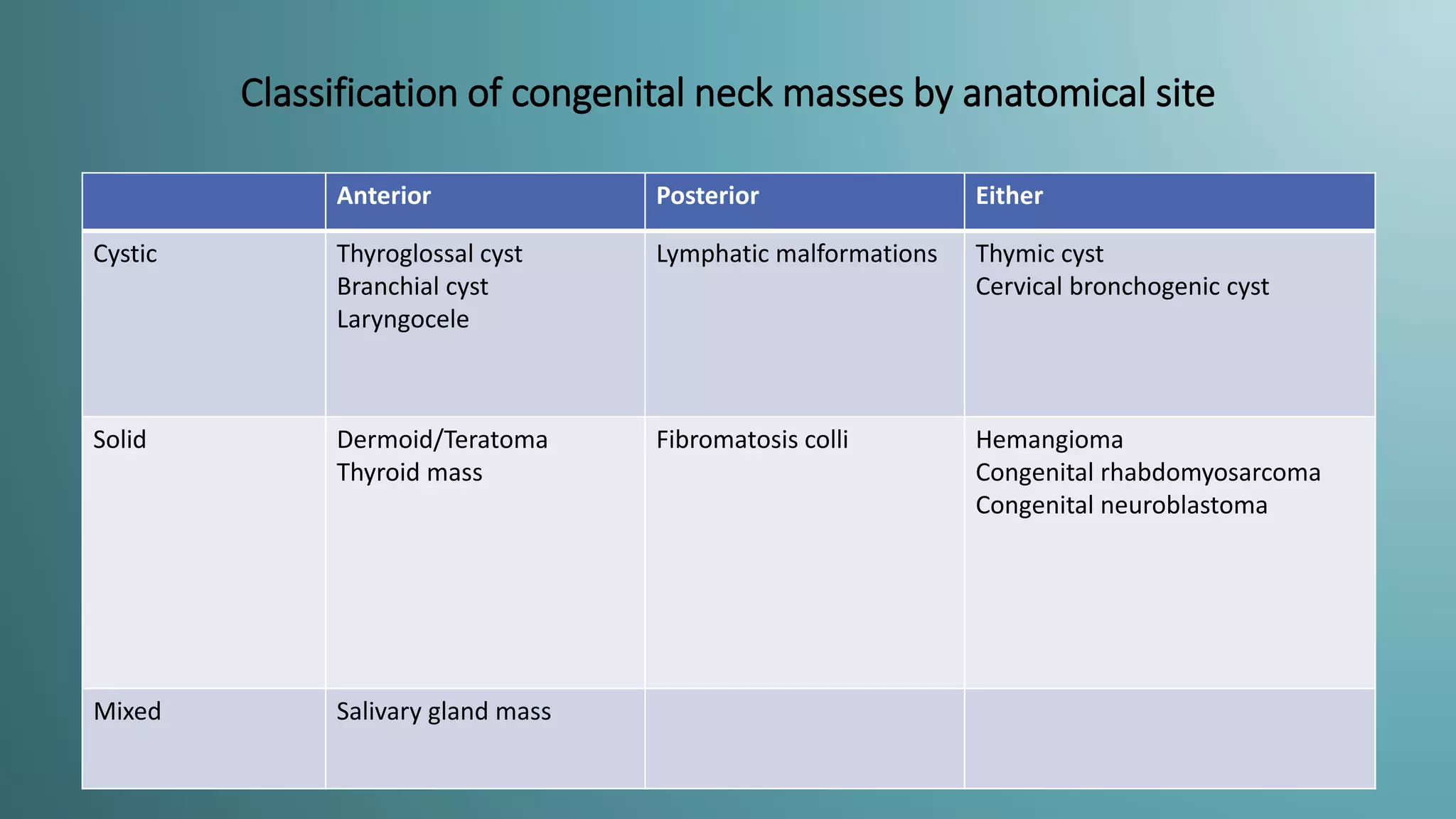
Cervical congenital neck masses are rare lesions primarily diagnosed in infants and children, often arising from developmental defects, mostly presenting as cystic formations. The document categorizes these masses by anatomical sites, discusses diagnostic imaging methods (USG, CT, MRI), and details specific types such as thyroglossal duct cysts, branchial cysts, and various tumors. It emphasizes the importance of accurate diagnosis for effective management and treatment of these conditions.