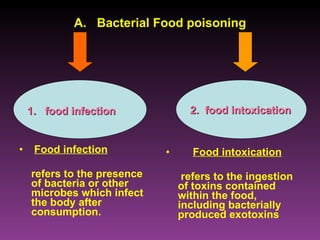
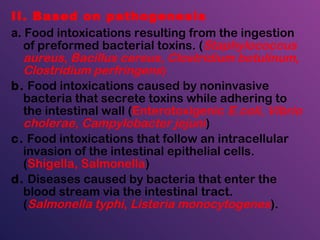
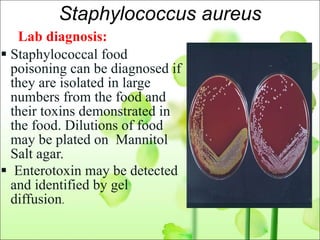
This document discusses bacterial food poisoning, describing common causative agents, symptoms, pathogenesis, and methods of diagnosis. The major bacterial causes outlined are Staphylococcus aureus, Bacillus cereus, Clostridium perfringens, Salmonella, Clostridium botulinum, and Escherichia coli. Symptom onset times and clinical manifestations are provided for classifying different types of food poisoning. The document also covers food contamination and poisoning prevention methods.