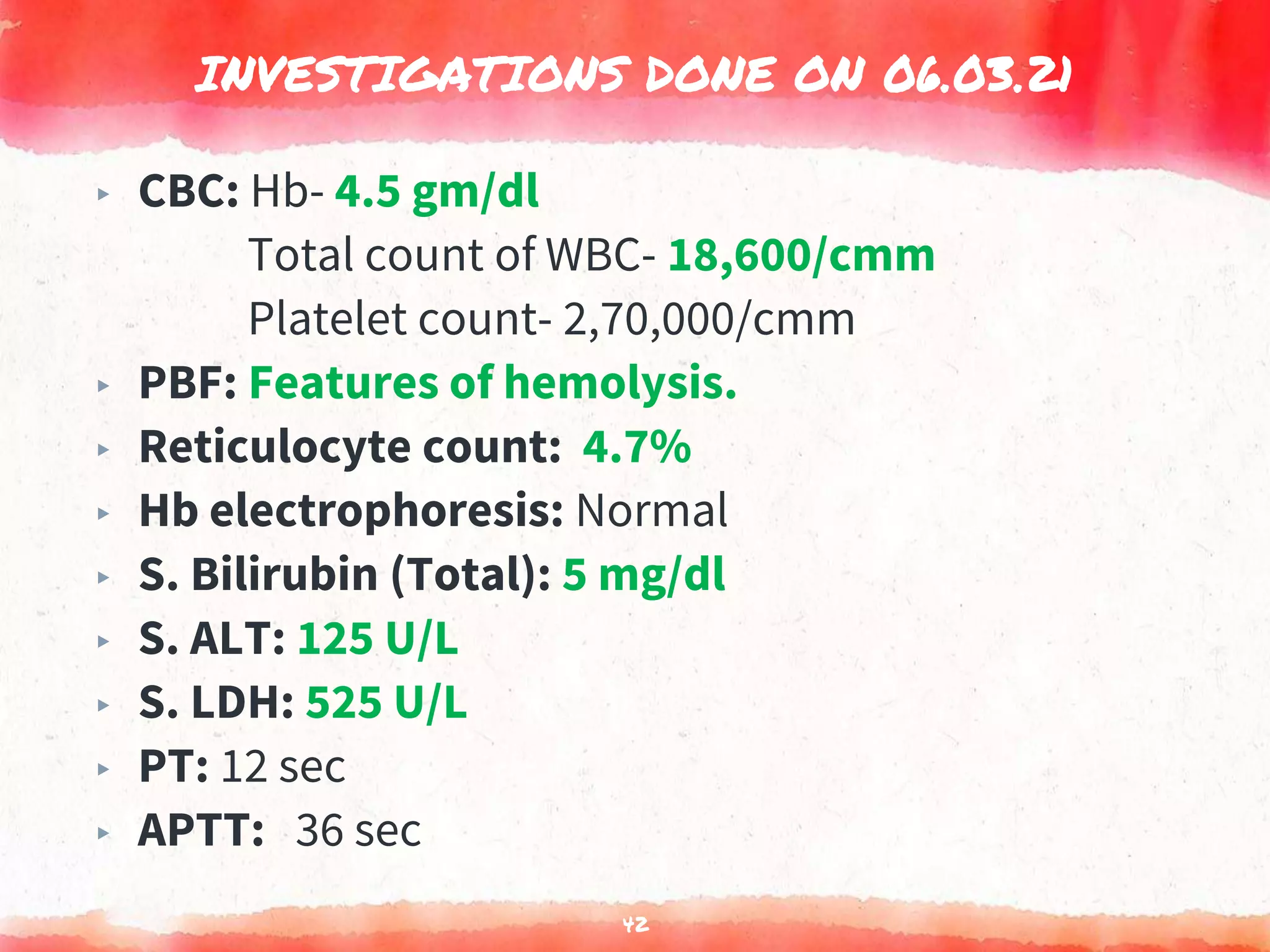
Alfi, a 10-year old boy, presented with sudden onset of severe pallor, dark colored urine, and jaundice. Examination found severe pallor, jaundice, splenomegaly, and otherwise normal vital signs. Initial workup showed features of hemolysis, positive direct Coombs test, and elevated bilirubin and LDH. The provisional diagnosis was autoimmune hemolytic anemia, which was confirmed. Treatment with steroids led to improvement in symptoms and laboratory values over subsequent follow ups.