10-year-old boy presented with abdominal pain, fever and vomiting for 3 days. On examination, he had tenderness in his abdomen. Initial tests showed elevated white blood cell count and CRP. Imaging found fluid in the pelvis and loaded colon. He was treated conservatively but his fever persisted. Further imaging found appendicitis, abscesses and bowel adhesions. He underwent laparoscopic appendectomy and drainage of abscesses. Pus culture was negative. His condition improved with antibiotics and supportive care and he was discharged after 16 days.













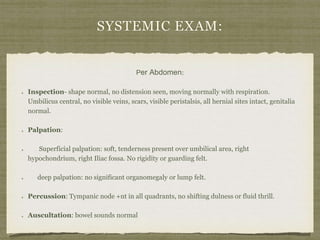



![day- 3
TEMP-101.7 F
hb-11.3
TLC-13000
CRP-24
Rx- Ceftriaxone+
Amikacin+
Metronidazole
0
1
2
94.5
96
97.5
99
100.5
102
103.5
11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26
day 1
TEMP-100.3 F
hb-11.3g%
TLC-16000
CRP-29
Platelets- 249 x 109/L
DLC- N87L7.2M4.3E0.6B0.2
BLOOD C/S- NIL
USG-FLUID IN
PELVIS,
LOADED
COLON
Rx- IV Ceftriaxone
Amikacin
metrogyl
Anti-pyretics
IV fluids
day- 7
TEMP-103 F
hb-10.6g%
TLC-16500
CRP-12.
S. Bilirubin- 0.3mg/dl
albumin- 2.8 mg/dl
bloodc/s- no growth
USG- gall bladder edema,
mild hepatitis
fluid collection in pelvis
viral markers- negative
Rx- Ceftriaxone+
Amikacin+
Metronidazole
day- 10
TEMP-99.1 F
hb-11.6g%
TLC-15000
CRP-6.9
X-ray Abdo-Multiple Air-fluid
Levels
CECT- INFLAMED APPENDIX,
SUB-HEPATIC ABSCESS,
INTRA-BOWEL ADHESIONS
AND THICKENING
SURGERY WAS PLANNED
Rx- Ceftriaxone+
Amikacin+
Metronidazole+
Piperacillin+ Tazobactam
day- 12
TEMP-102 F
Pus Gram stain- no organism
Pus c/s- no growth
Rx- Ceftriaxone+
Amikacin+
Metronidazole+
Meropenem
VANCOMYCIN ADDED
FEVER
[in deg F]
day- 11
TEMP-99.9 F
DIAGNOSTIC LAP DONE
Rx- Ceftriaxone+
Amikacin+
Metronidazole+
ALLERGIC TO PIPTAZ SO
MEROPENEM ADDED
day- 16
TEMP-98 F
ORAL INTAKE
IMPROVED
DISHARGED
NOVEMBER 2017](https://image.slidesharecdn.com/unit2fridaycase-180711153952/85/appendicitis-v-s-enteric-fever-20-320.jpg)

