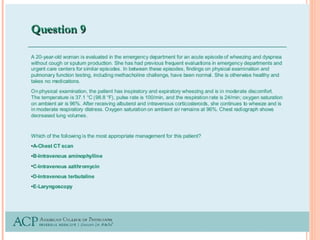
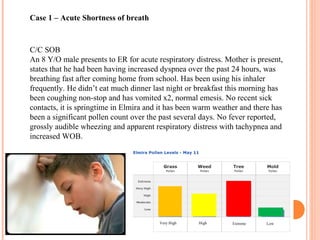
An 8-year-old male presents to the emergency room with acute shortness of breath likely due to an asthma exacerbation. His symptoms have been worsening over the past 24 hours. On examination, he has increased work of breathing and wheezing. Arterial blood gas shows respiratory acidosis. He is started on nebulized bronchodilators and steroids to treat the exacerbation.
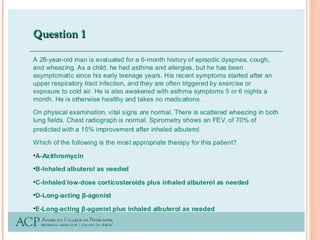
A 24-year-old male presents to clinic with worsening cough, wheezing, and dyspnea over the past 3 days in the setting of an upper respiratory infection. Examination reveals wheezing. He is diagnosed with an asthma exacerbation from his upper respiratory symptoms and started on inhaled

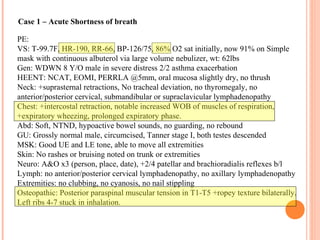








![THE 4 STAGES OF BLOOD GAS PROGRESSION IN PERSONS WITH
STATUS ASTHMATICUS ARE AS FOLLOWS:
STAGE 1 - CHARACTERIZED BY HYPERVENTILATION WITH A
NORMAL PARTIAL PRESSURE OF OXYGEN (PO 2)
STAGE 2 - CHARACTERIZED BY HYPERVENTILATION
ACCOMPANIED BY HYPOXEMIA (IE, A LOW PARTIAL PRESSURE OF
CARBON DIOXIDE [PCO 2] AND LOW PO 2)
STAGE 3 - CHARACTERIZED BY THE PRESENCE OF A FALSE-
NORMAL PCO 2; VENTILATION HAS DECREASED FROM THE
HYPERVENTILATION PRESENT IN THE SECOND STAGE; THIS IS AN
EXTREMELY SERIOUS SIGN OF RESPIRATORY MUSCLE FATIGUE
THAT SIGNALS THE NEED FOR MORE INTENSIVE MEDICAL CARE,
SUCH AS ADMISSION TO AN ICU AND, PROBABLY, INTUBATION
WITH MECHANICAL VENTILATION.
STAGE 4 - CHARACTERIZED BY A LOW PO 2 AND A HIGH PCO 2,
WHICH OCCURS WITH RESPIRATORY MUSCLE INSUFFICIENCY;
THIS IS AN EVEN MORE SERIOUS SIGN THAT MANDATES
INTUBATION AND VENTILATORY SUPPORT.
Status Asthmaticus workup, Medscape
http://emedicine.medscape.com/article/2129484-workup#aw2aab6b5b4](https://image.slidesharecdn.com/4c423385-6f57-4a3a-b349-db1fdaec5fb4-150526201242-lva1-app6891/85/Asthma-14-320.jpg)