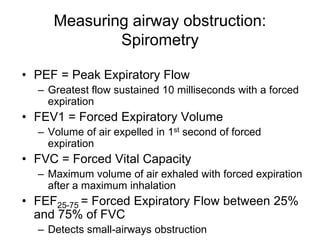
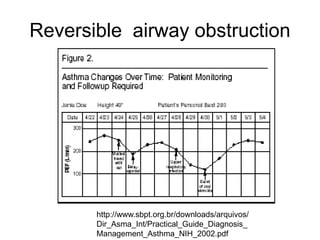
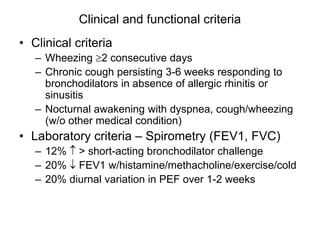
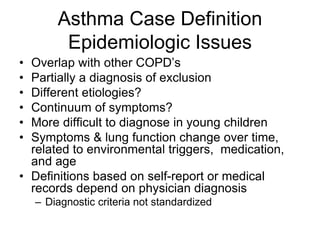
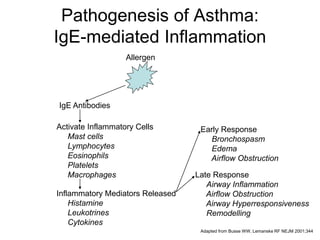
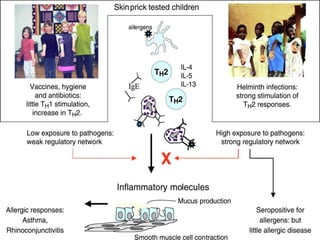
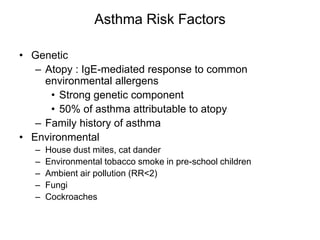
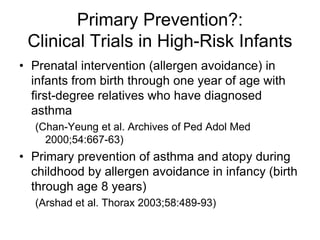
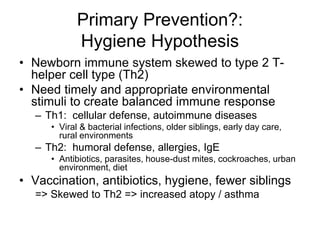
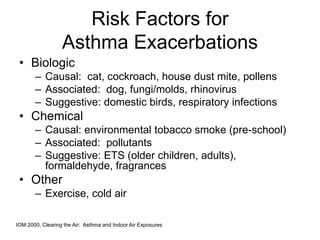
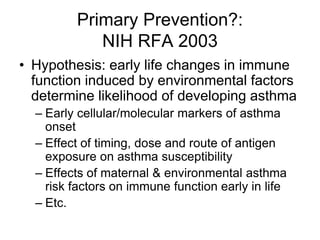
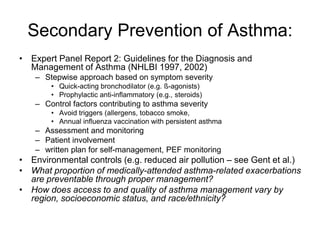
Asthma is a chronic lung disease characterized by reversible airway obstruction and airway inflammation. It can be triggered by various environmental factors and allergens. Diagnosis involves measuring lung function through spirometry and checking for improvements after bronchodilator use. Prevention strategies aim to reduce exposure to triggers through environmental controls and allergen avoidance. Treatment follows guidelines that use medication on a stepwise basis depending on symptom severity. Despite treatment, exacerbations still occur and disproportionately impact some groups, highlighting the need for improved management across populations.