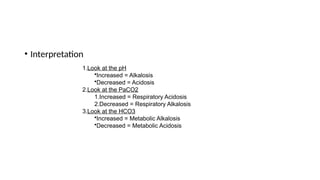
The document outlines essential concepts in the care of critically ill patients, defining critical illness and critical care, and emphasizing a multidisciplinary approach to management. It details the three main categories of ICU patient management, including ventilatory and hemodynamic support, treatment of specific illnesses, and preventive care, along with various monitoring techniques such as arterial blood gas analysis and hemodynamic monitoring. Key considerations for effective care include rapid assessment, appropriate therapy delivery, and maintaining patient safety through protocols and the 'fast hug' concept.









![Ct’
[5]](https://image.slidesharecdn.com/thecriticallyiilpatientbasicconcepts-240815183313-40c749f1/85/The-Critically-iil-patient-Basic-concepts-pptx-15-320.jpg)