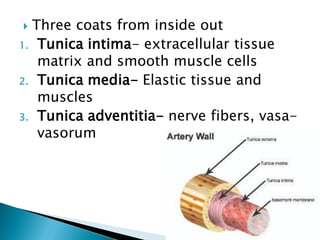
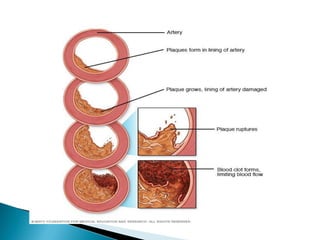
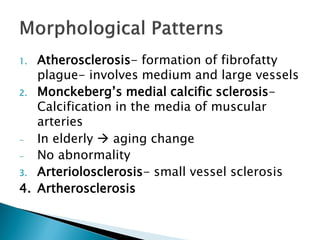
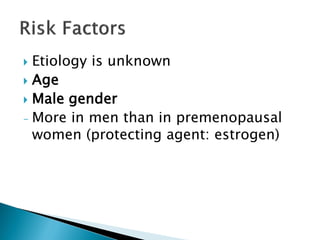
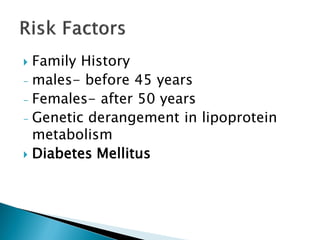
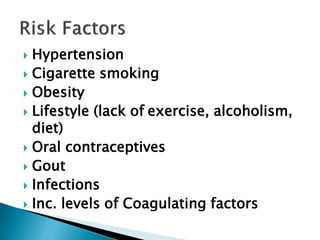
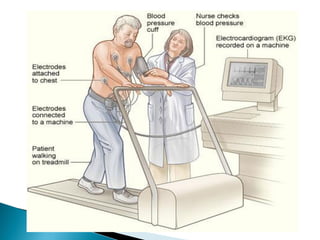
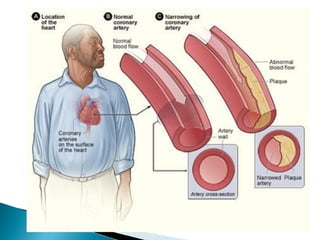
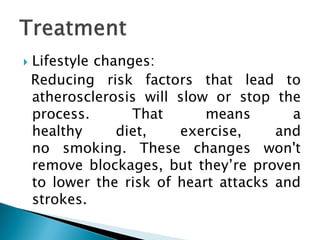
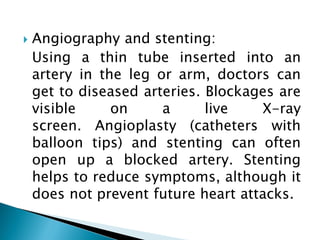
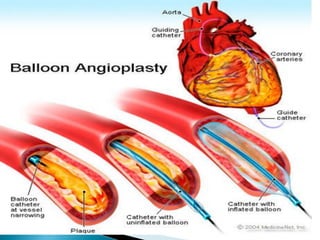
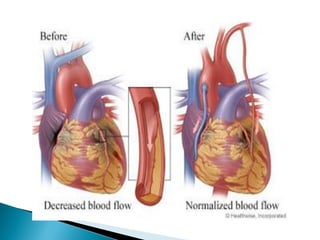
This document discusses arteriosclerosis and atherosclerosis. It defines arteriosclerosis as the hardening and thickening of arteries. Atherosclerosis is a specific type of arteriosclerosis where plaque builds up in the arteries due to an inflammatory response. The document outlines the structure of arteries, risk factors for atherosclerosis such as smoking and diabetes, symptoms of atherosclerosis like chest pain, and treatments including lifestyle changes, medication, surgery, and stenting.