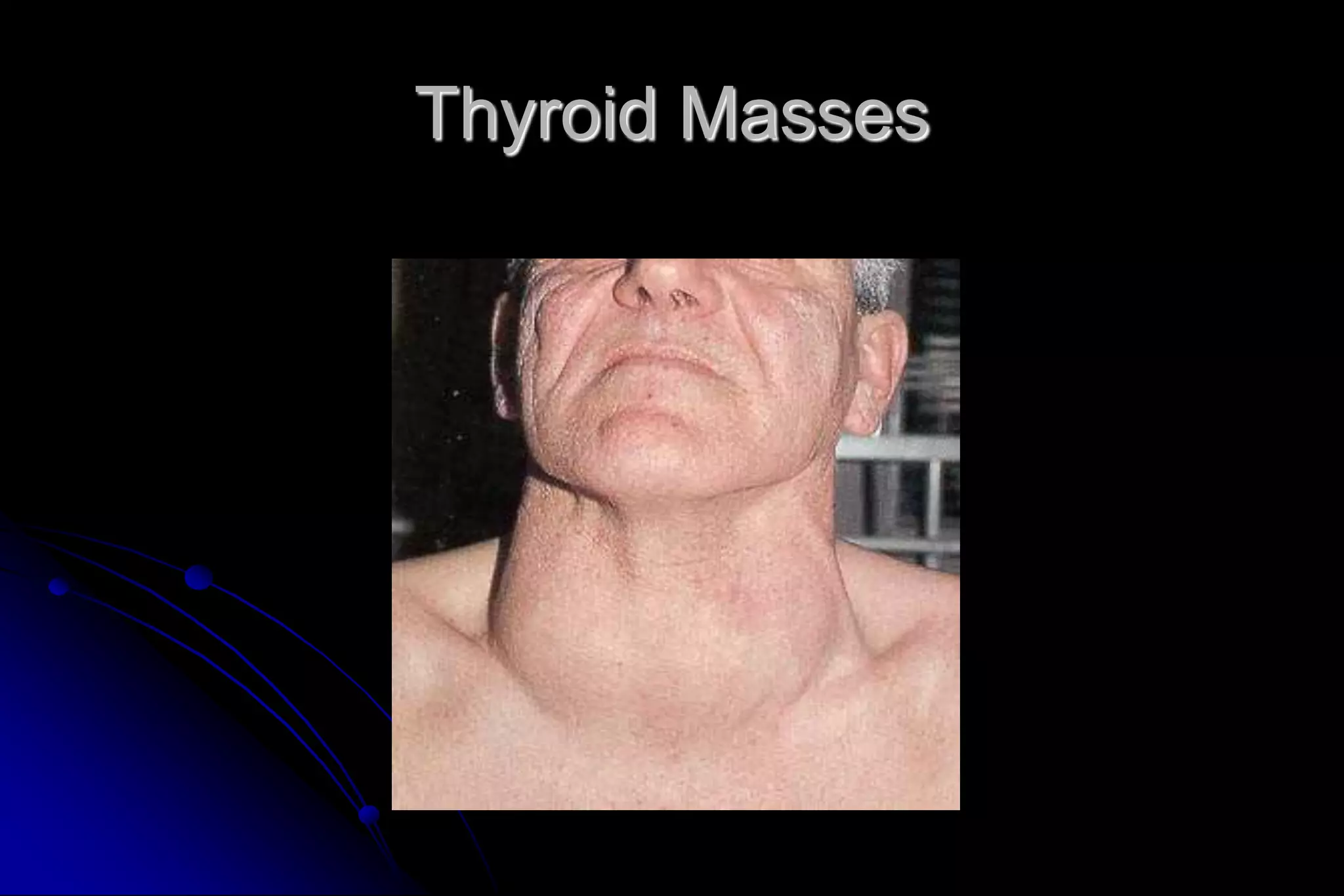
This document provides guidance on evaluating neck masses, which have a complex differential diagnosis across all age groups. It outlines important anatomical landmarks and recommends a systematic approach starting with history, exam, and fine needle aspiration biopsy to characterize the mass. Common etiologies include thyroid masses, lymphadenopathy, salivary gland tumors, and vascular or neurogenic lesions. In children, inflammatory causes are more likely while malignancy is a greater concern in adults. Otolaryngologists play an important role in diagnosing and managing these conditions.