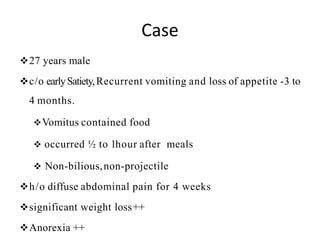
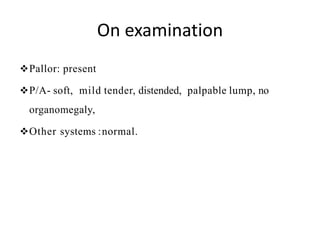
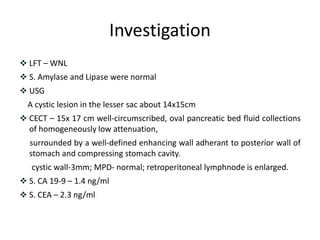
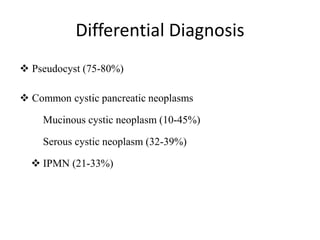
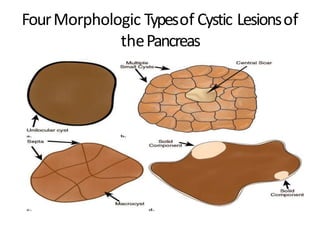
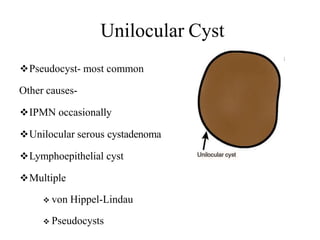
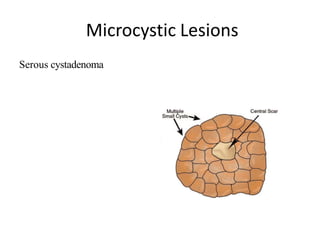
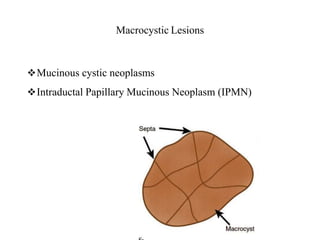
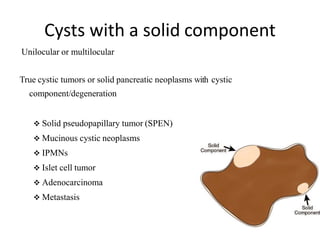
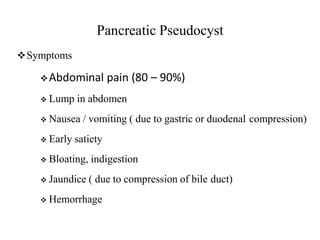
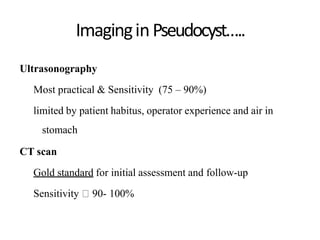
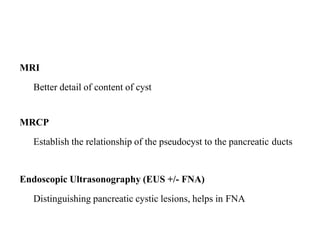
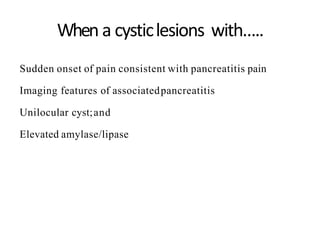
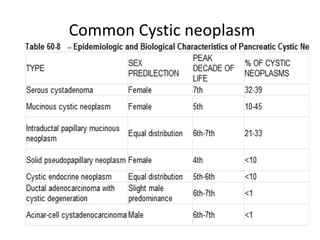
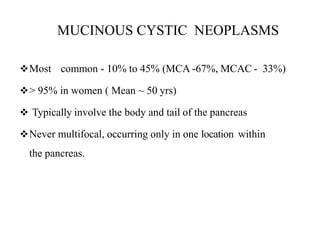
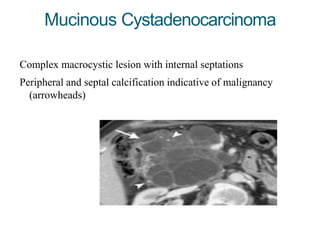
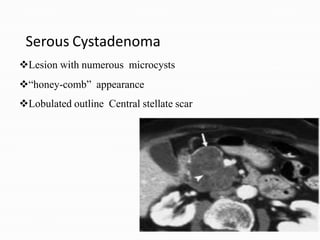
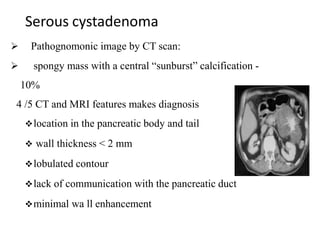
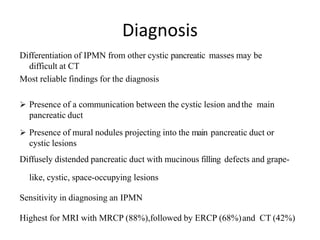
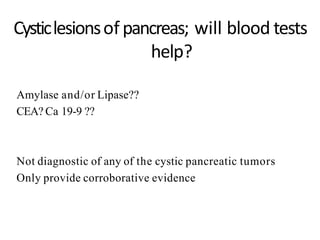
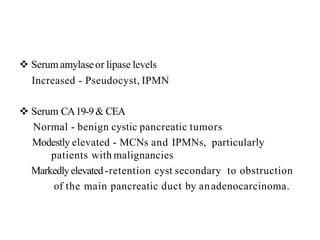
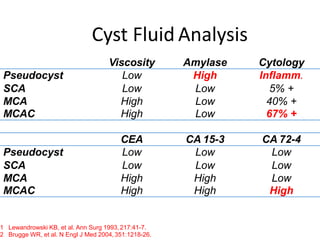
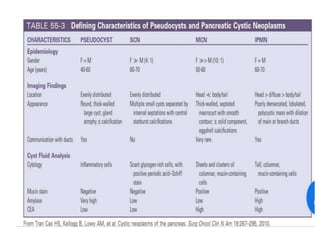
A 27-year-old male presented with early satiety, recurrent vomiting, weight loss, and abdominal pain. Imaging revealed a large cystic lesion in the pancreas. Differential diagnoses for cystic pancreatic lesions include pseudocyst, serous cystadenoma, mucinous cystic neoplasm, and intraductial papillary mucinous neoplasm. Based on the presentation of abdominal pain following episodes of alcohol use and imaging findings of a well-defined cystic lesion surrounded by an enhancing wall, this case is most consistent with a pancreatic pseudocyst.