This document provides information on several pediatric hip conditions:
1) Developmental dysplasia of the hip (DDH) is a dysplasia or dislocation of the hip that develops in infants, and can range from shallow acetabulum to complete dislocation. It occurs in approximately 1 in 1000 live births and is more common in females.
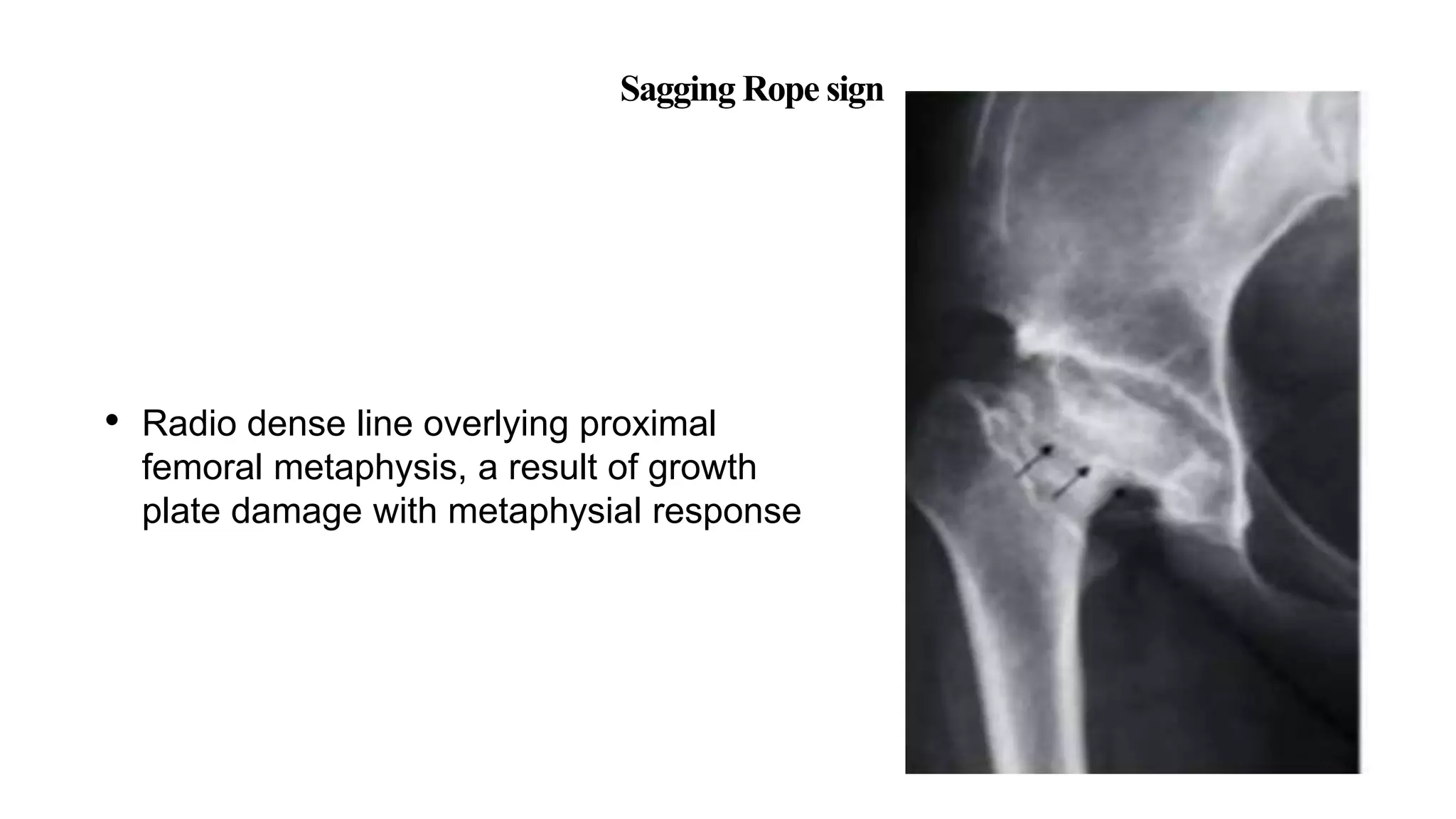
2) Perthes disease is a disorder of the hip that affects children ages 4-8, causing the death of bone in the femoral head. It presents with limping, groin pain, and decreased range of motion.
3) Slipped capital femoral epiphysis (SCFE) is a slip of the femoral epiphysis relative to the femoral neck