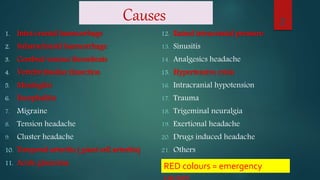
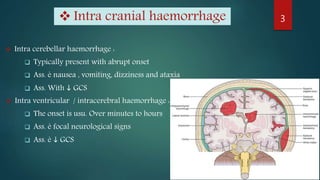
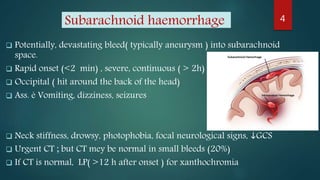
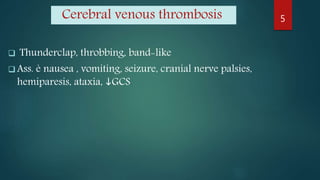
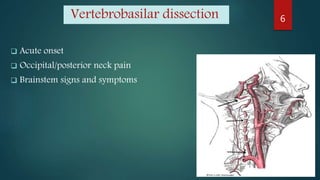
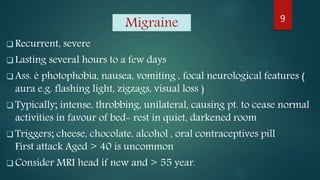
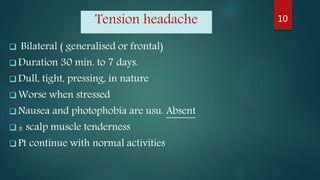
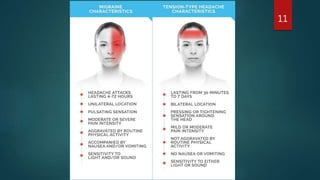
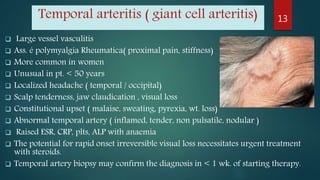
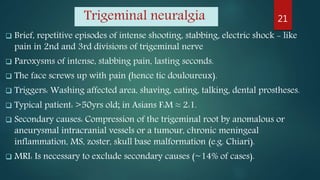
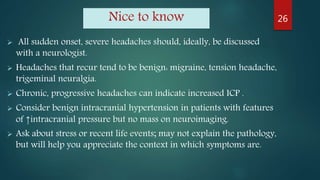
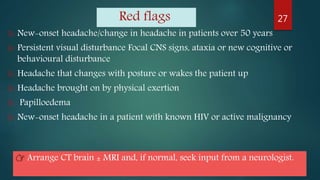
The document provides a comprehensive overview of various causes of headaches, including serious conditions such as intracranial hemorrhages, meningitis, and vascular disorders, alongside common types like migraine, tension, and cluster headaches. It emphasizes the importance of recognizing red flags for urgent conditions, especially in patients over 50 and highlights the need for diagnostic imaging in certain cases. The document serves as a guide for identifying headache types and applicable treatment options.