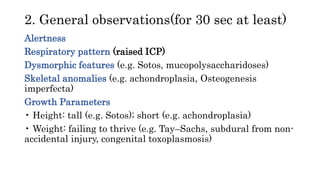
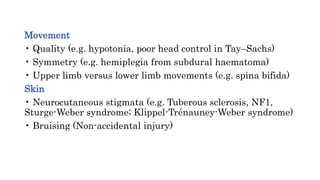
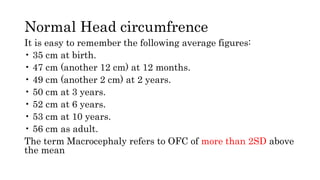
The document outlines an approach for examining a child with macrocephaly, detailing necessary observations and assessments including developmental milestones, neurological signs, and specific measurements. It emphasizes the importance of a methodical examination of the head, eyes, limbs, and other systems to identify potential underlying conditions. Key recommendations include measuring the head circumference multiple times, considering parental head sizes, and examining for signs of associated abnormalities.


![The most important things to remember in
this case:
1. Always measure the head yourself, until a constant result around the largest
diameter
is obtained (usually three times is enough).
2. Always measure the parents’ heads (in a similar fashion).
3. Always request the progressive percentiles of the child (parents’ charts unavailable).
4. Always examine the back, to avoid missing spinal dysraphism.
5. Always examine the lower limbs before the upper limbs, as the lower limbs are
first affected in hydrocephalus, because the tracts supplying them run closer to the
ventricles.
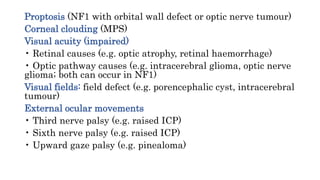
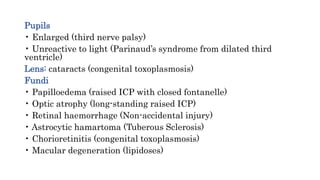
6. Always examine the eye movements, in particular the upward gaze (for Parinaud
syndrome, from raised intracranial pressure [ICP] compressing the mesencephalic
tectum/superior colliculus) and lateral rectus function (for raised ICP compressing
the sixth nerve).](https://image.slidesharecdn.com/approachtoachildwithlargehead-210702232655/85/Approach-to-a-child-with-large-head-20-320.jpg)