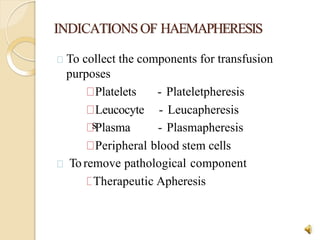
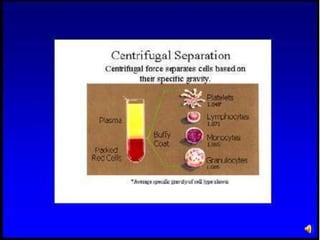
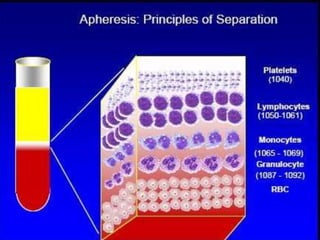
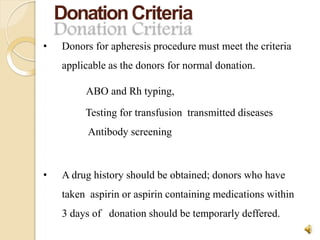
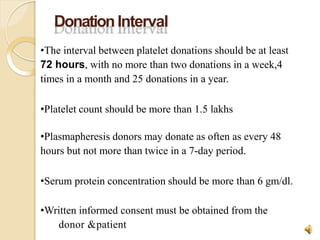
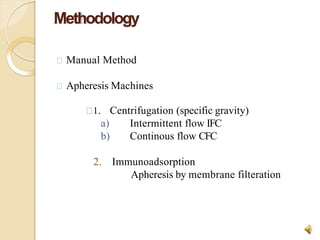
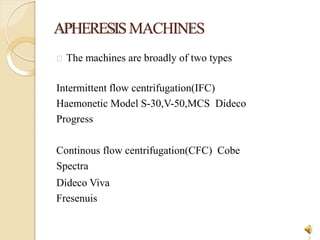
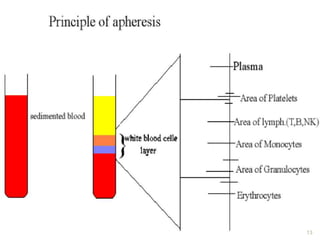
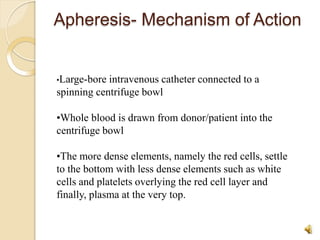
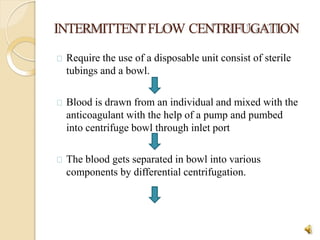
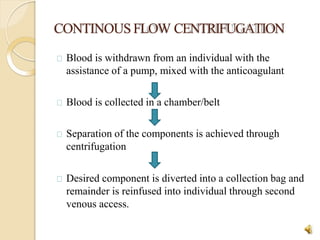
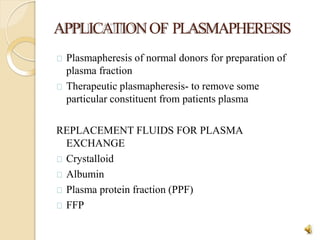
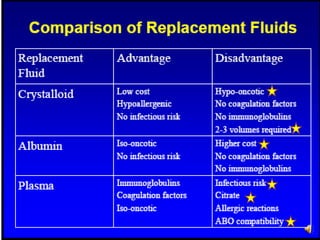
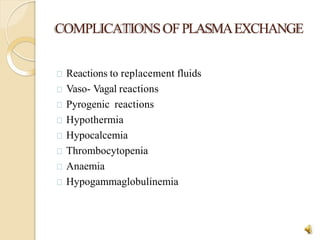
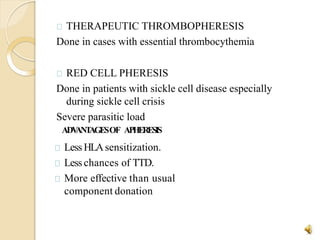
Apheresis is a technique where whole blood is collected from a donor or patient and separated into its components. The desired component is retained while the remaining constituents are returned. It is used to collect blood components for transfusion or remove pathological components. There are two main types of apheresis machines - intermittent flow centrifugation and continuous flow centrifugation. The process involves drawing blood, separating components via centrifugation, and collecting the desired component while returning the rest. Complications can include citrate toxicity, allergic reactions, and hypotension. Apheresis provides benefits over regular blood donation such as less HLA sensitization and lower risk of transfusion-transmitted infections.