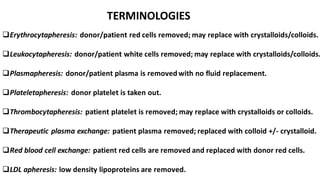
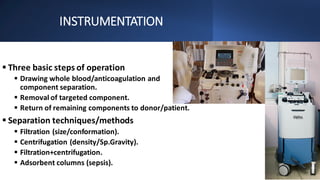
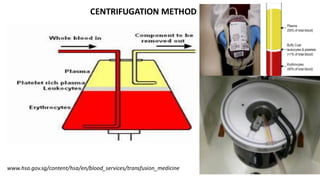
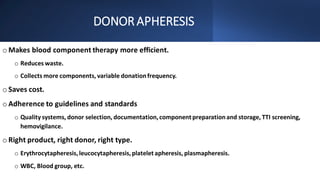
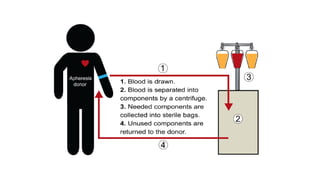
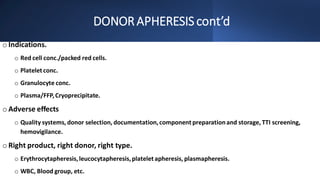
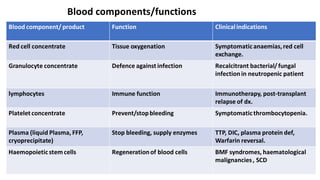
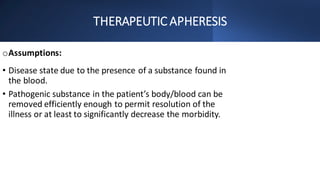
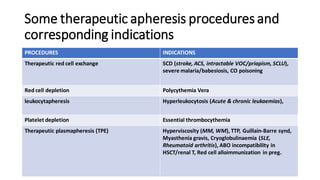
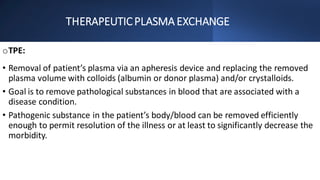
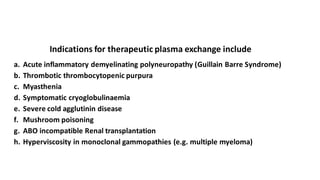
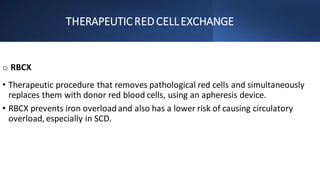
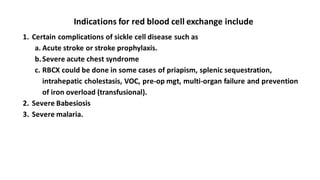
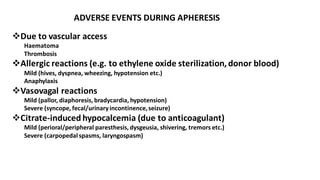
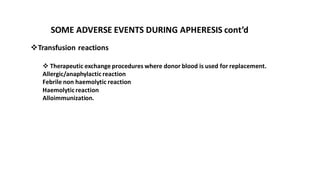
Apheresis is a process where blood components are separated and selectively removed. There are two main types - donor apheresis, where components are collected from healthy donors, and therapeutic apheresis, where pathogenic substances are removed from patients. Instrumentation involves drawing whole blood, separating components using centrifugation or filtration, and returning remaining components. Therapeutic apheresis procedures include plasma exchange, red blood cell exchange, and leukapheresis which are used to treat various conditions by removing pathological substances from the blood. Complications can occur due to vascular access, allergic reactions, or citrate toxicity from anticoagulants used.