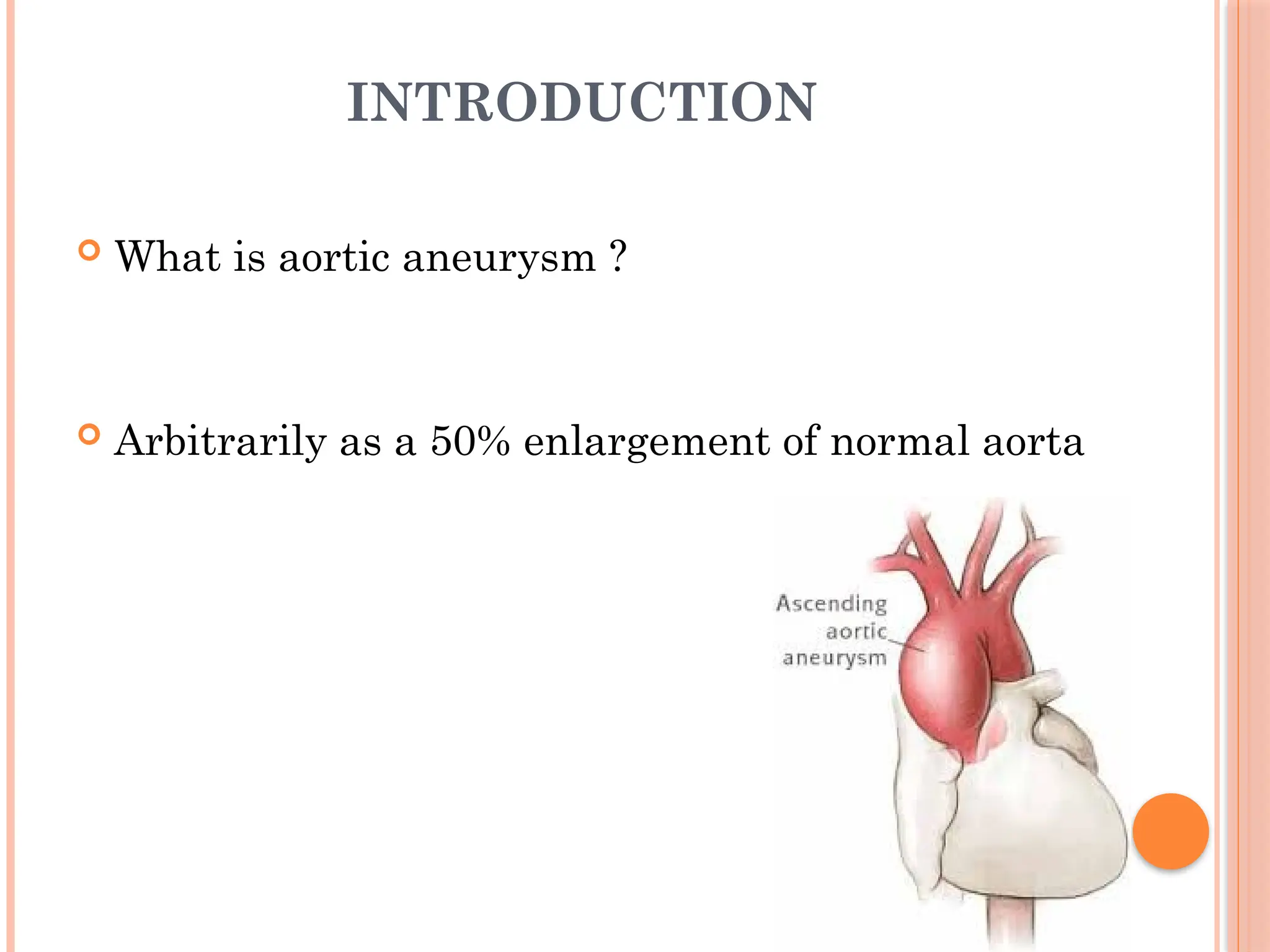
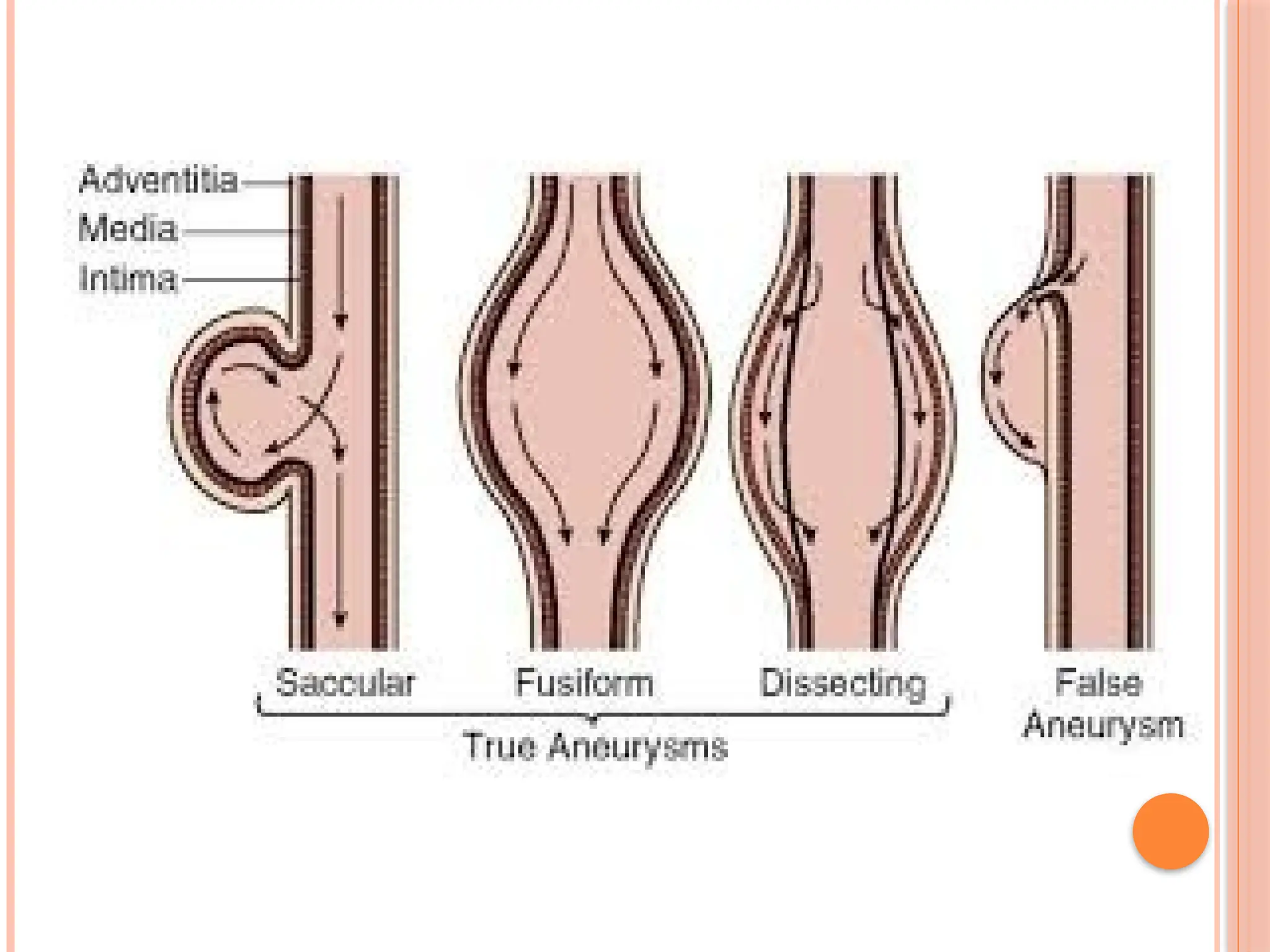
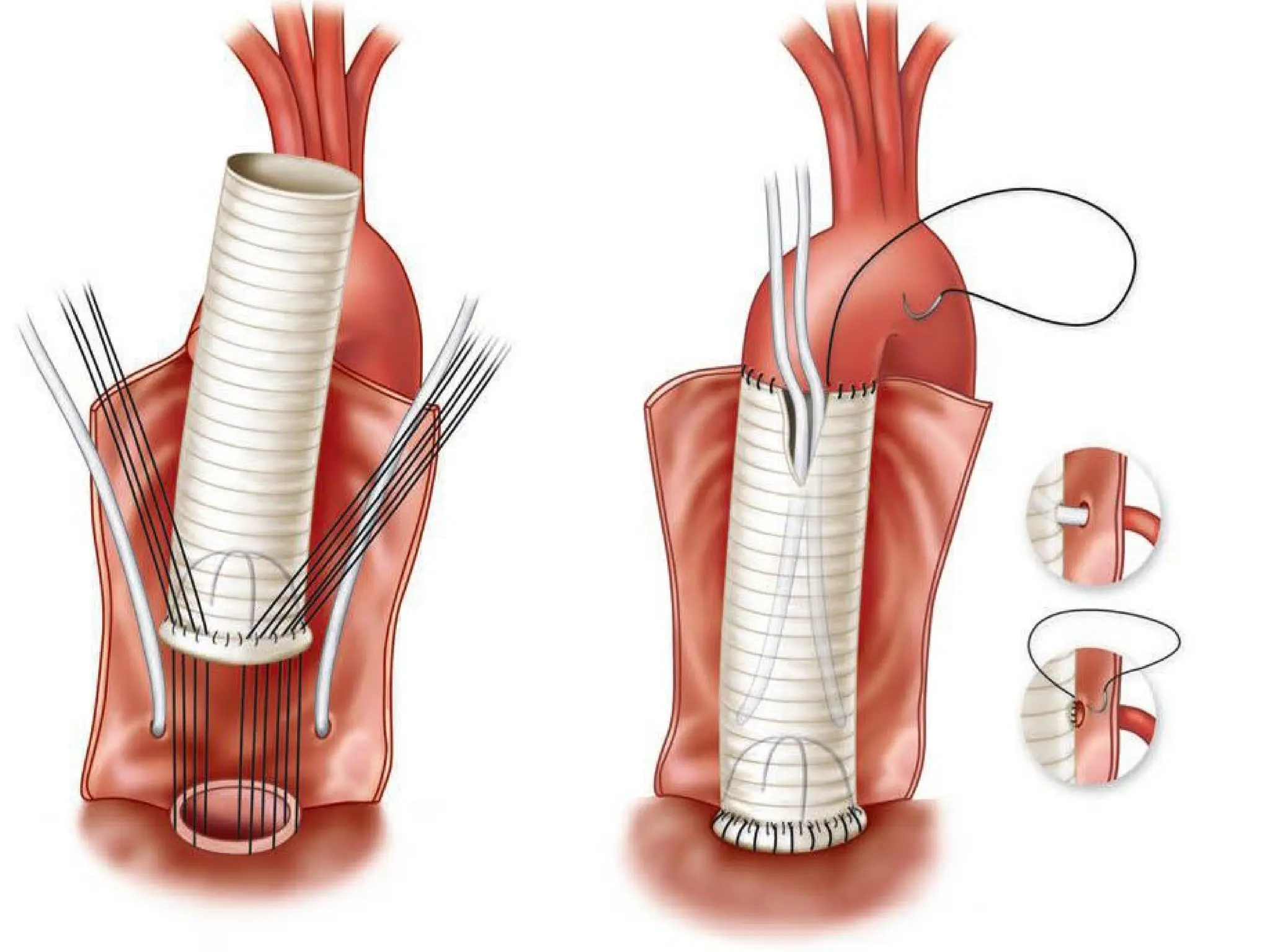
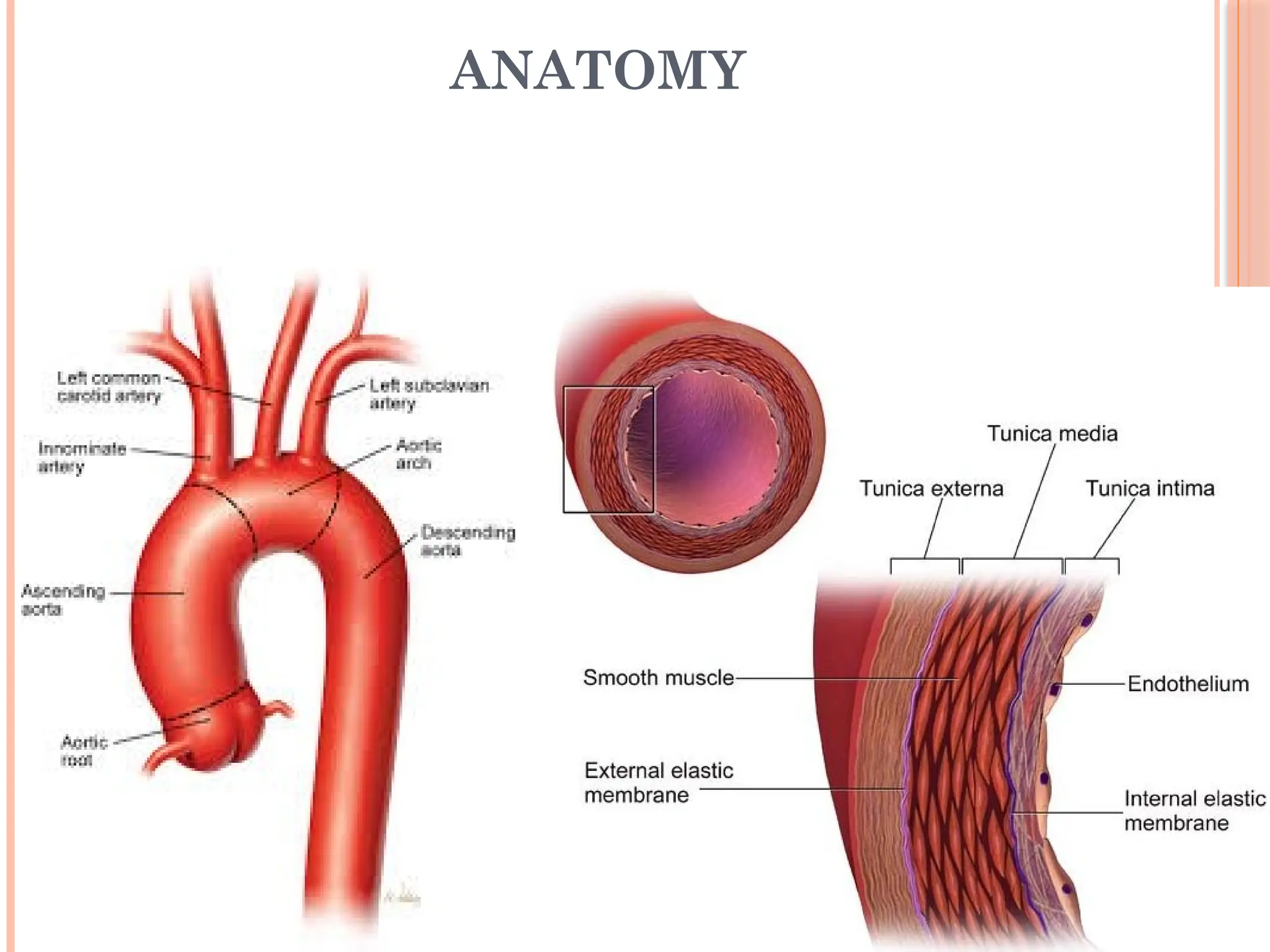
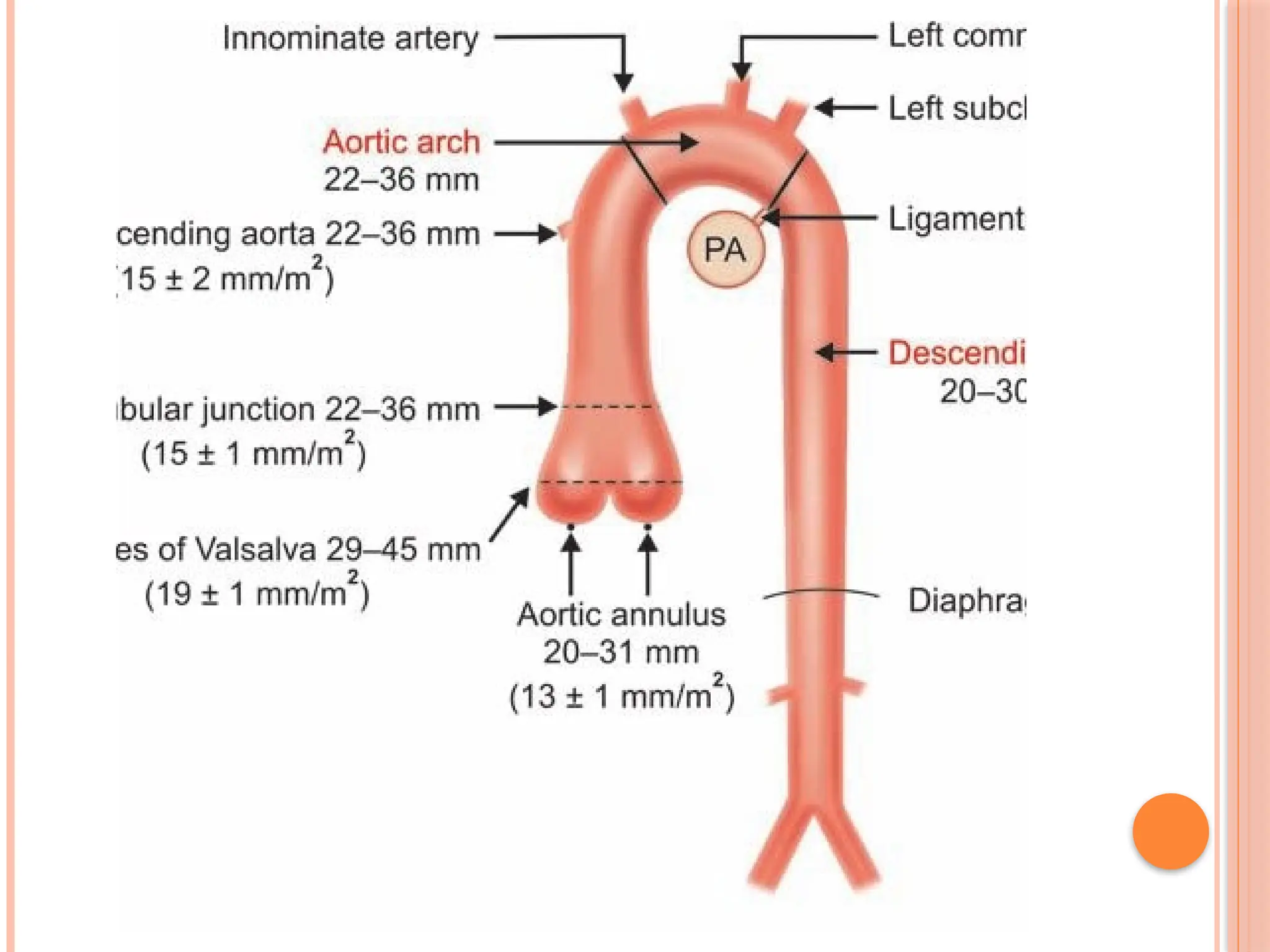
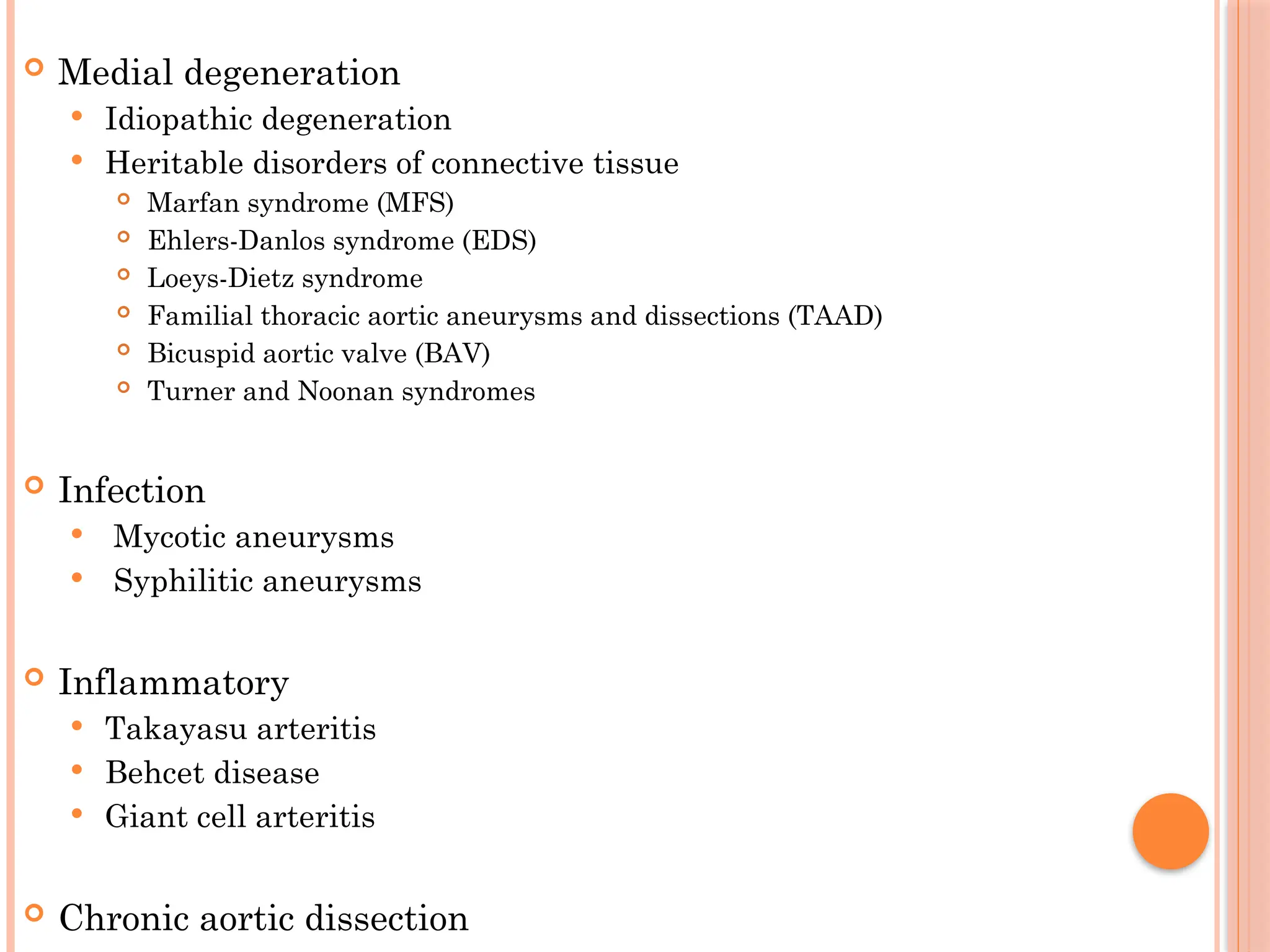
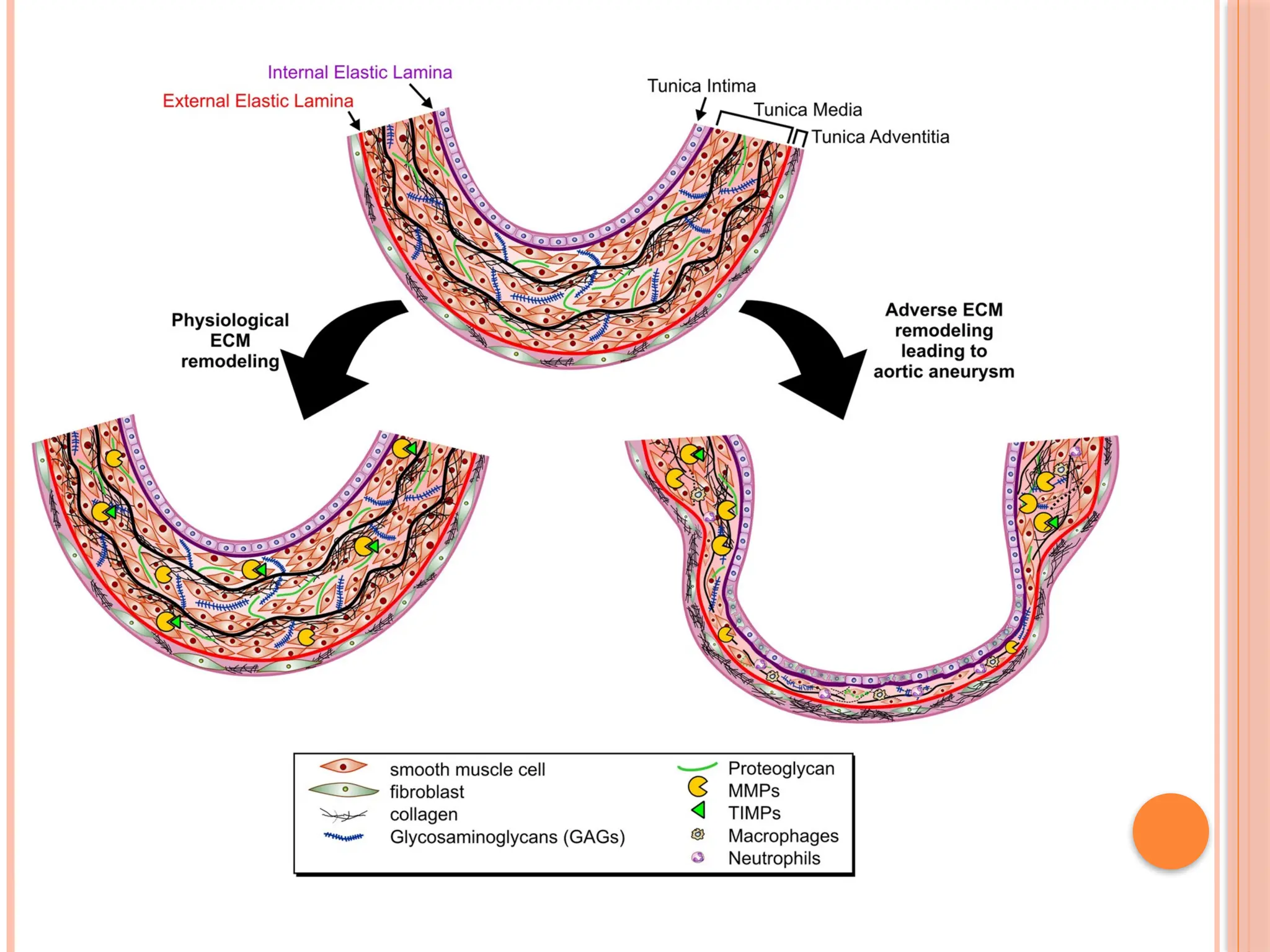
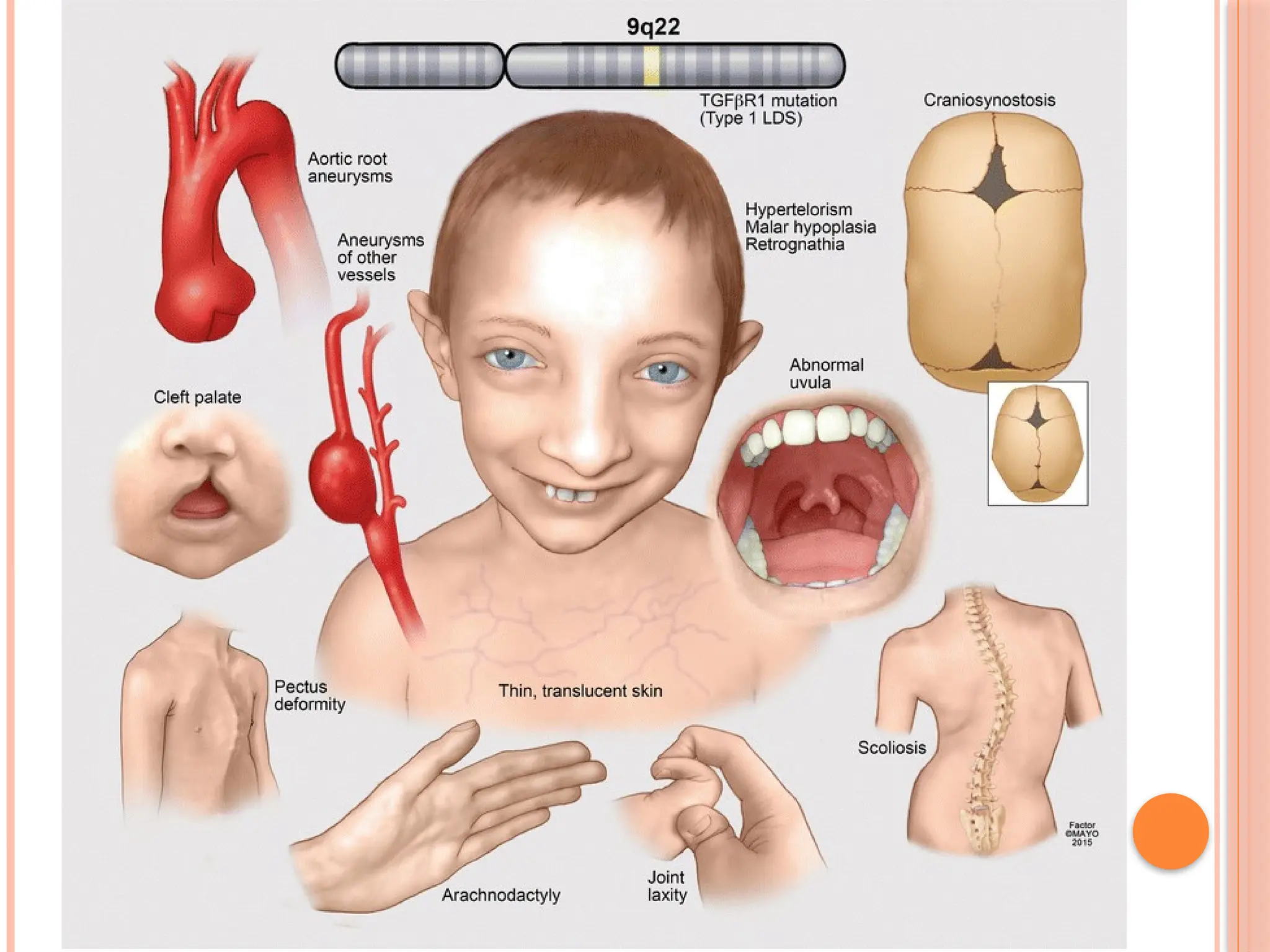
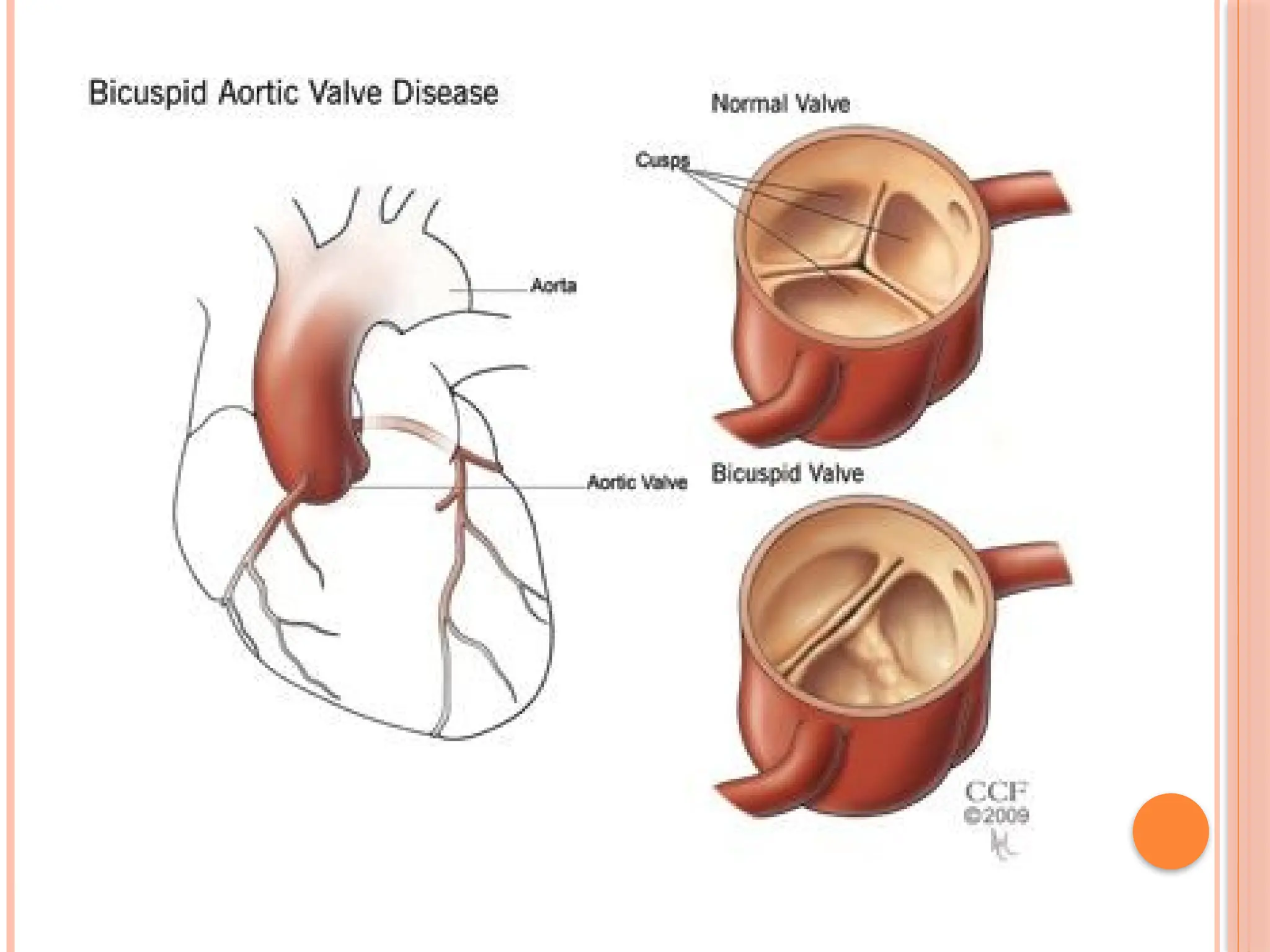
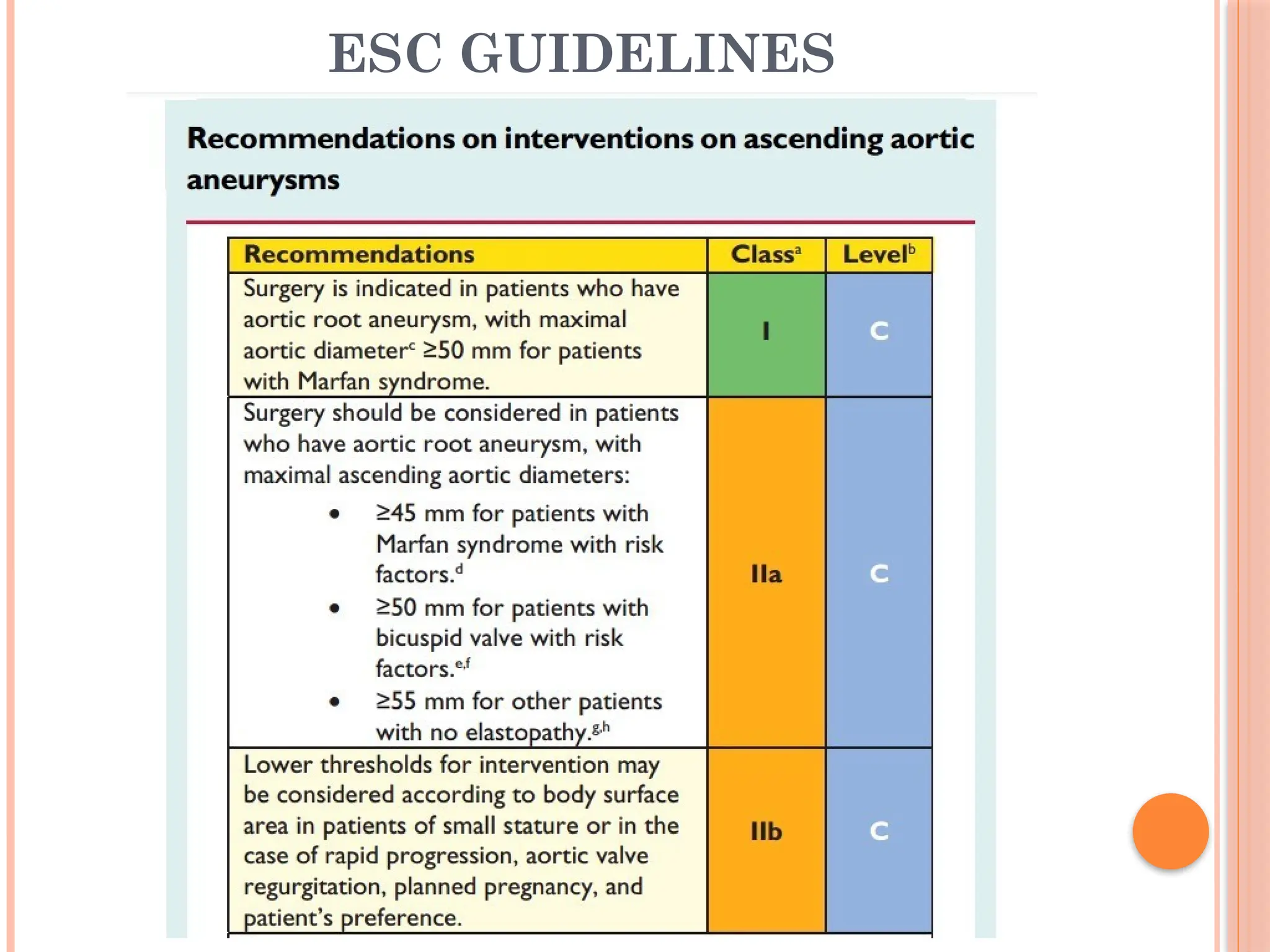
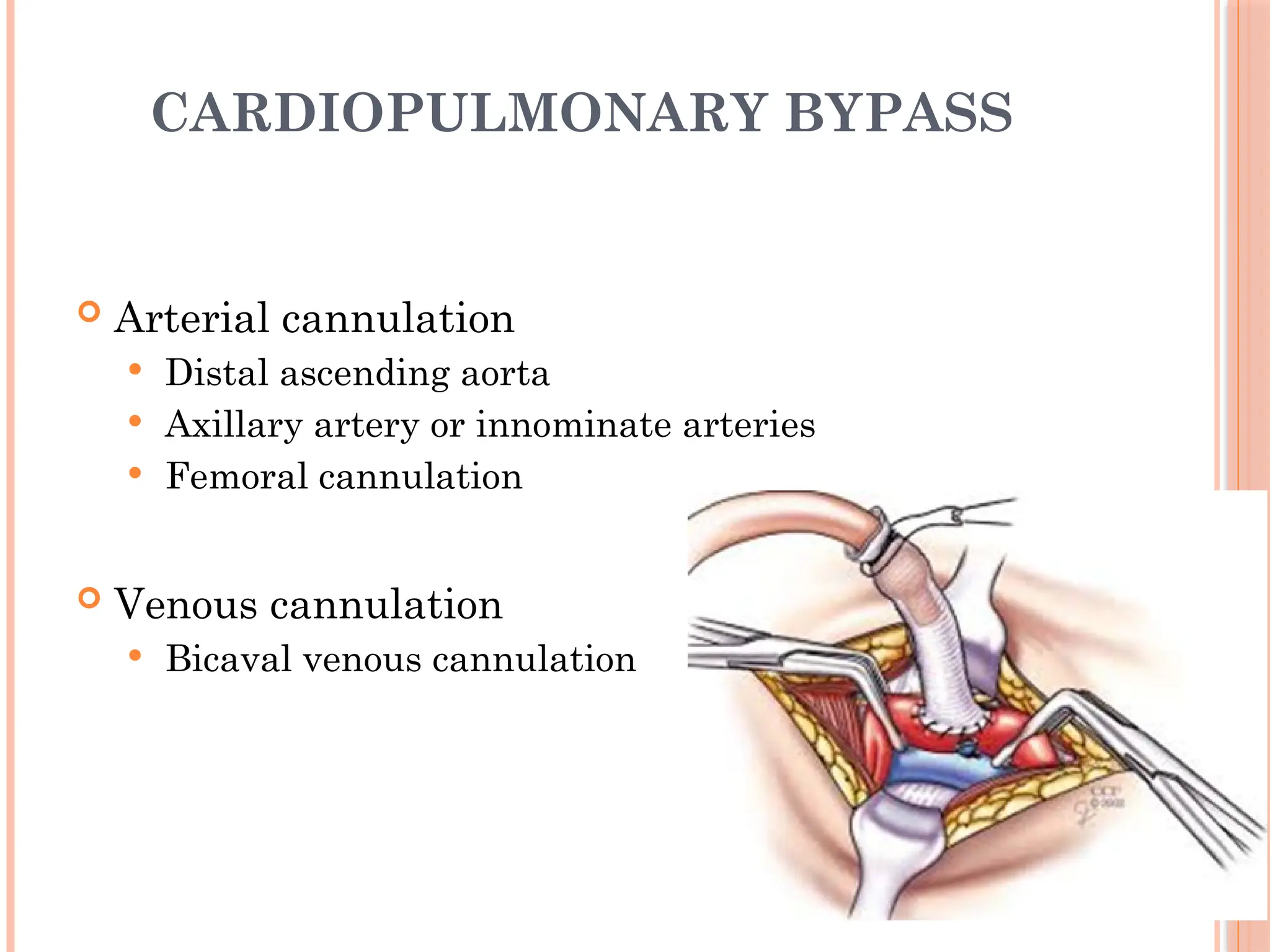
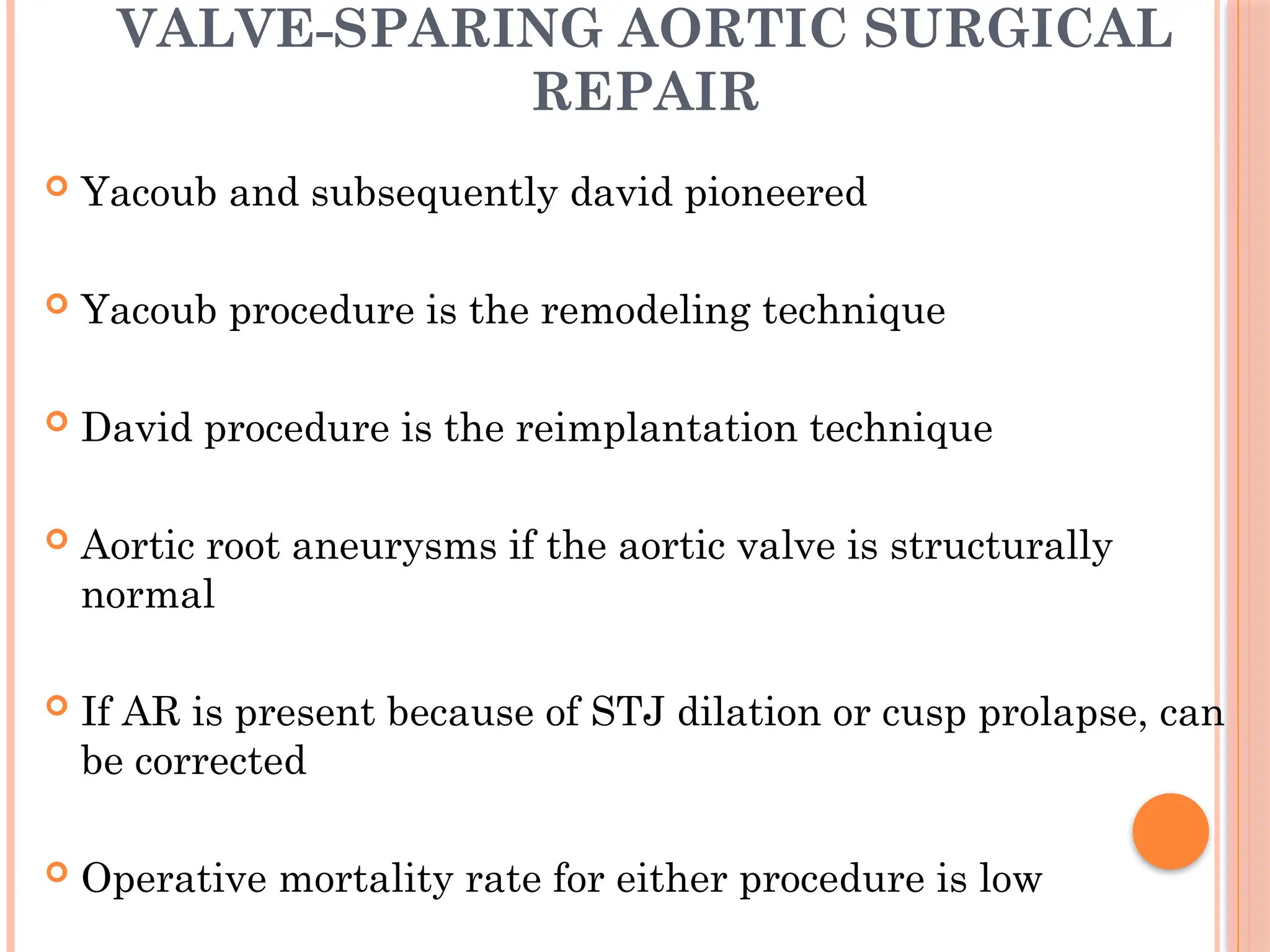
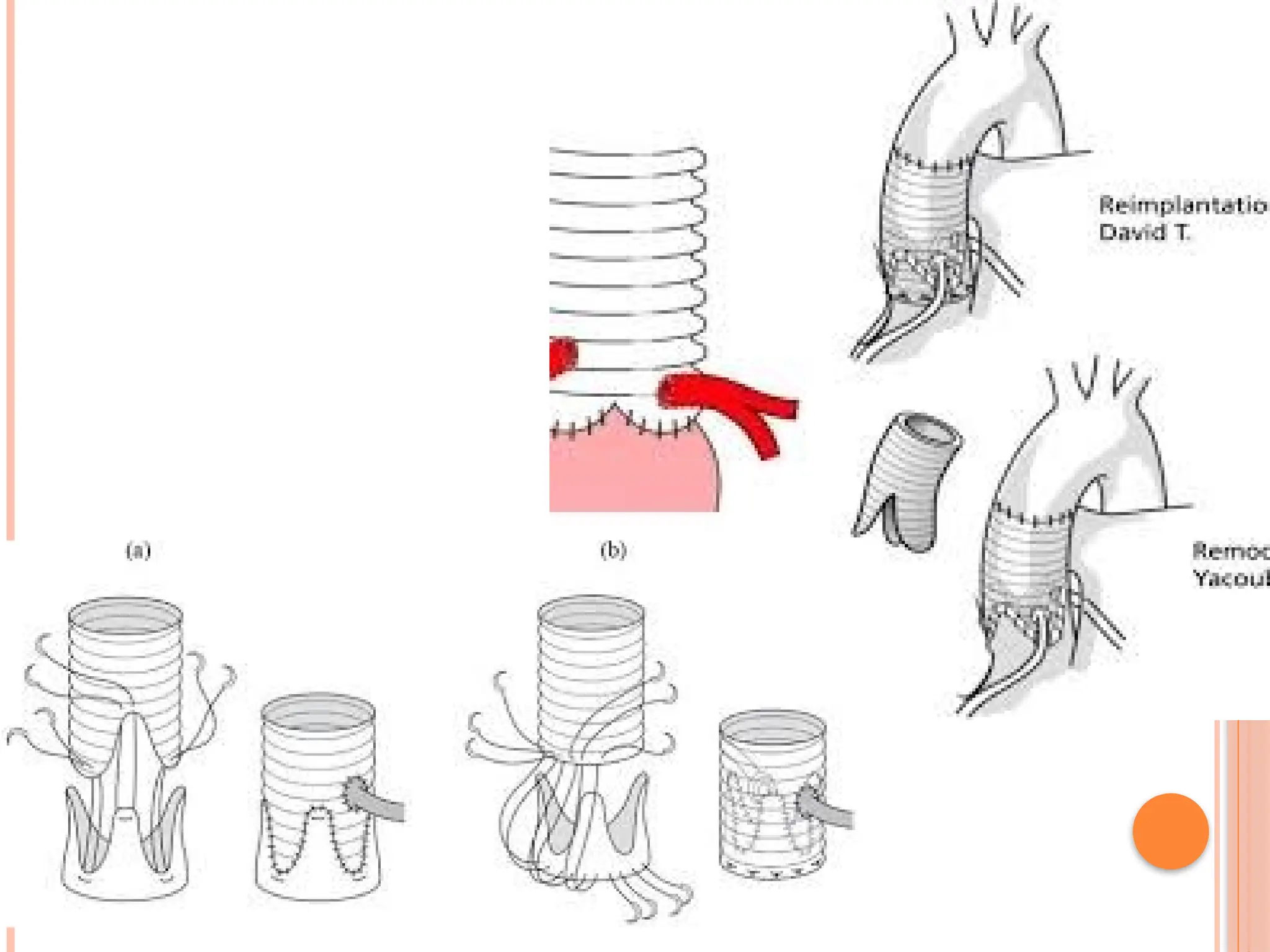
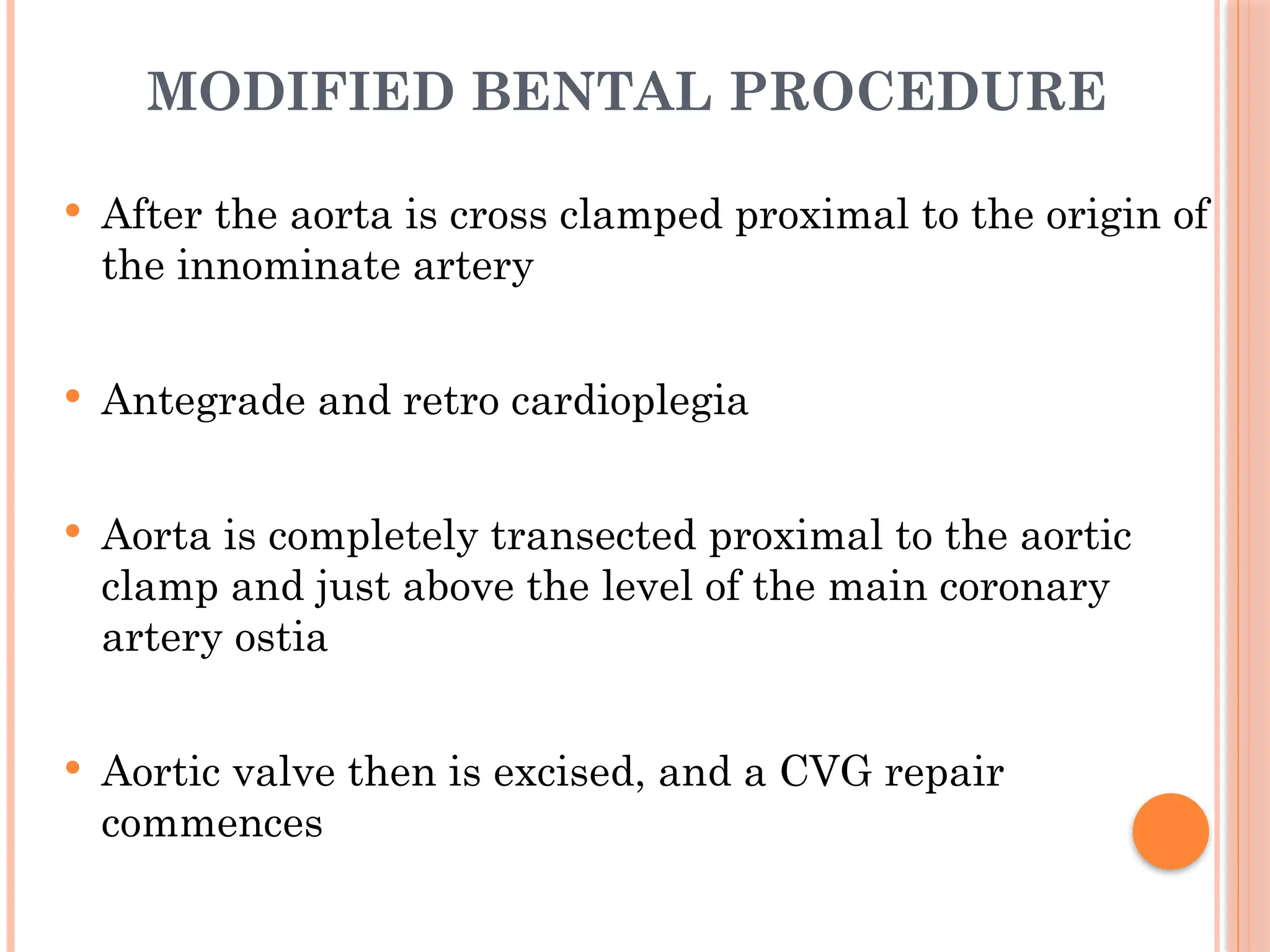
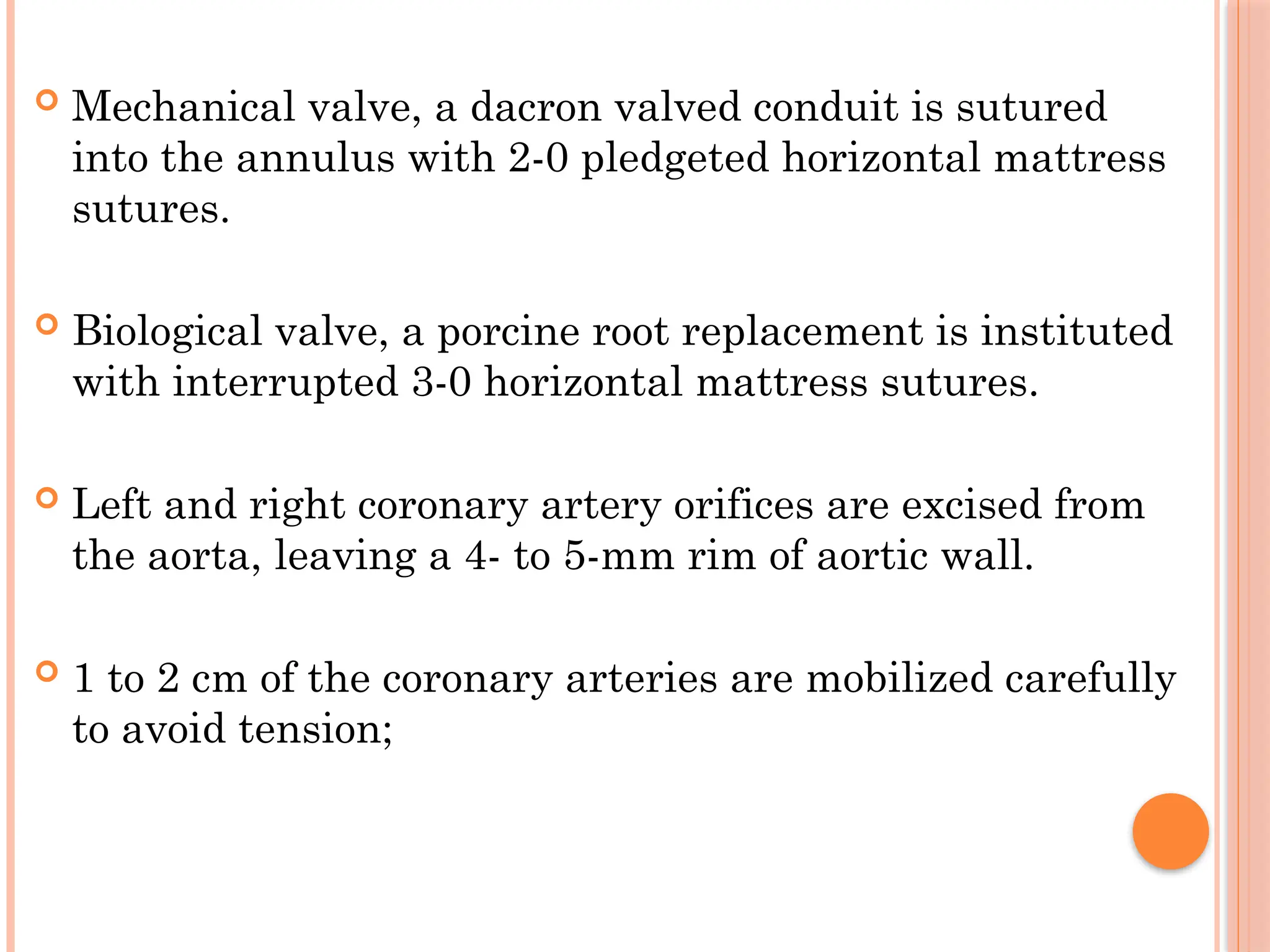
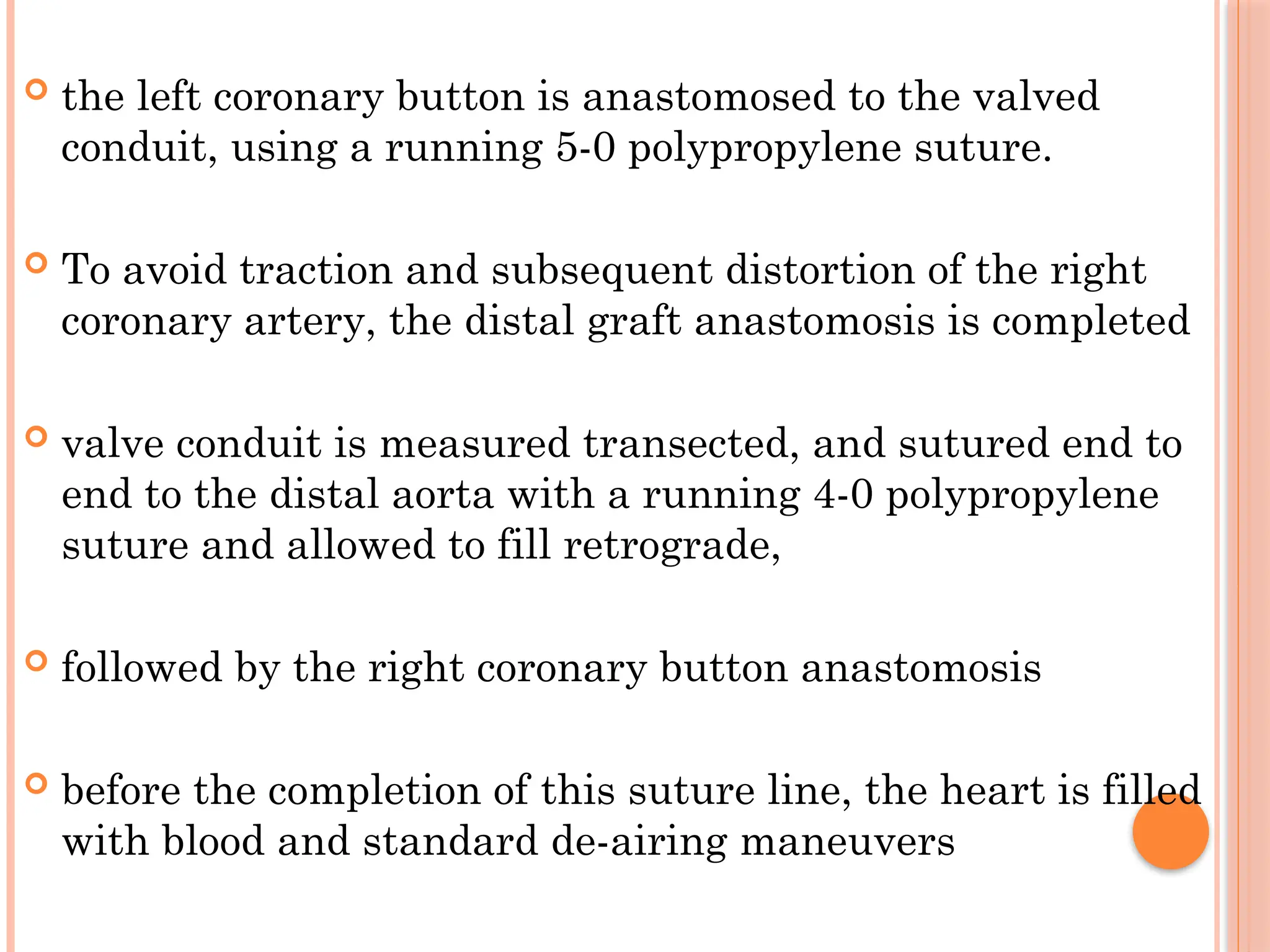
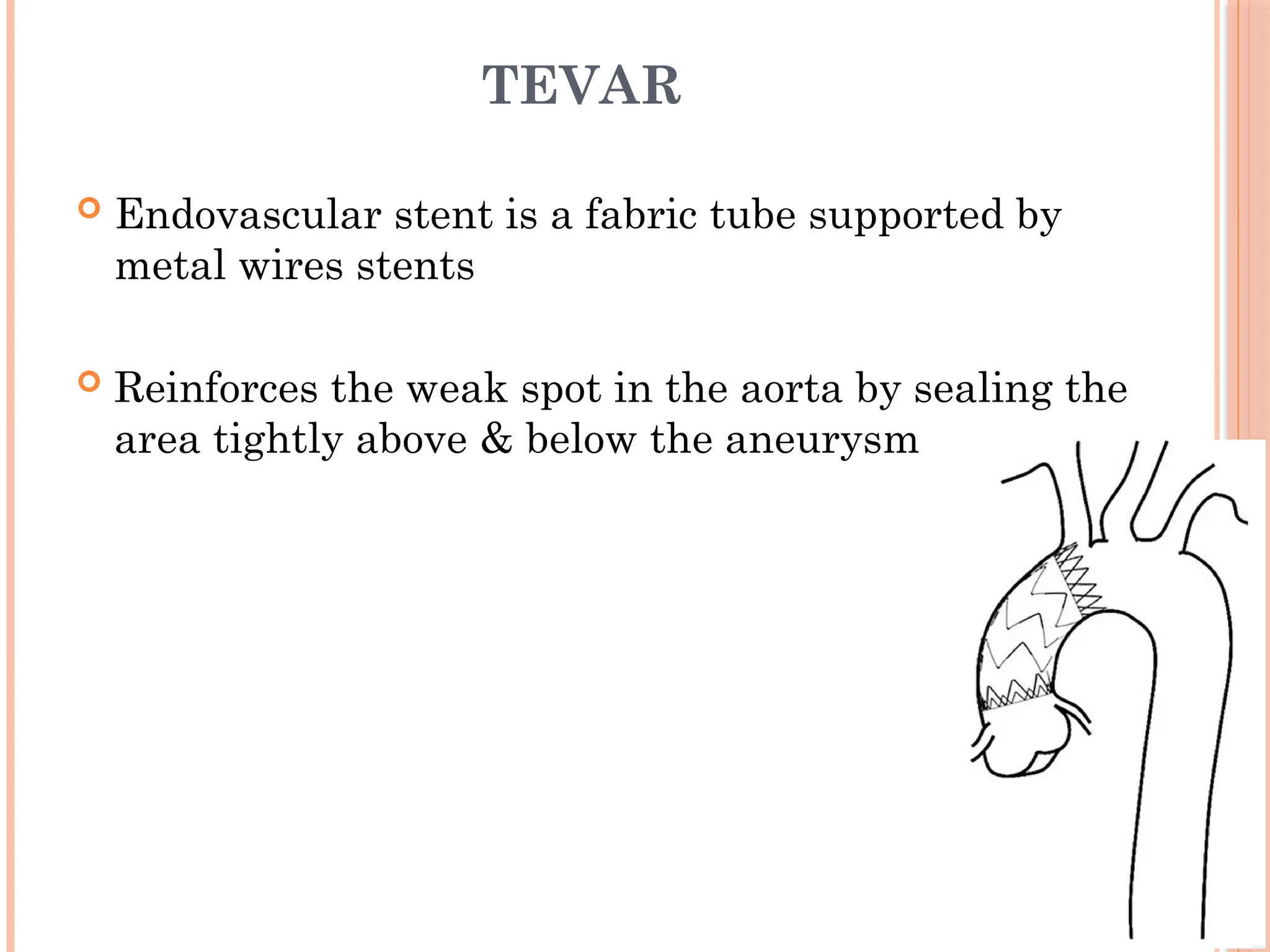
The document provides a comprehensive overview of ascending aortic aneurysms, detailing definitions, historical context, classifications, risk factors, and pathophysiology. It discusses specific genetic conditions associated with aneurysms, diagnostic methods, and management strategies, including both medical and surgical interventions. Additionally, the document addresses the implications of different surgical procedures and considerations for patient care.