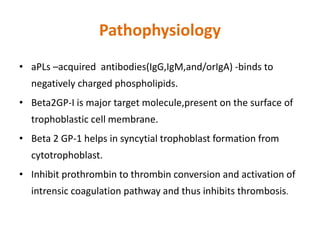
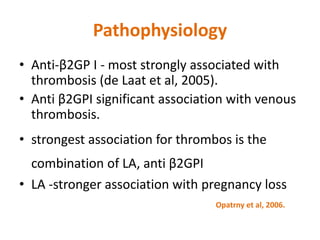
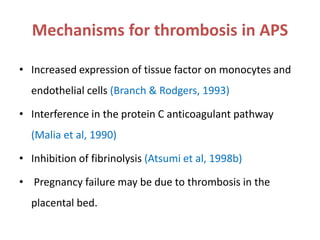
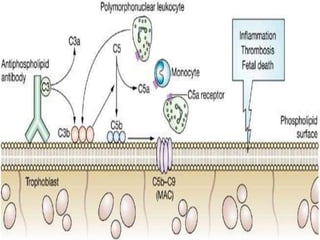
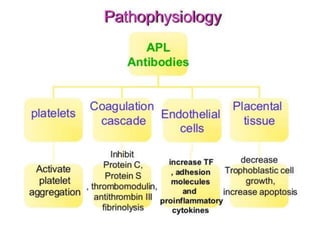
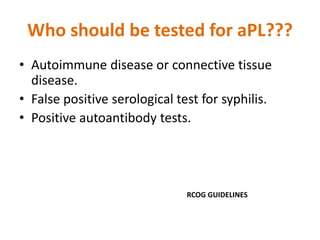
This document discusses antiphospholipid syndrome (APS), also known as Hughes syndrome. It is an autoimmune disorder associated with acquired thrombophilia. The key points are:
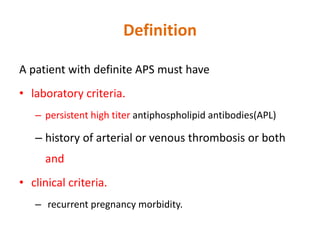
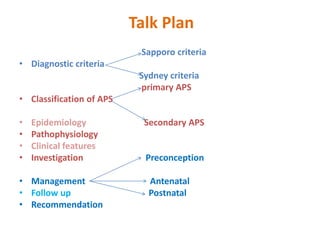
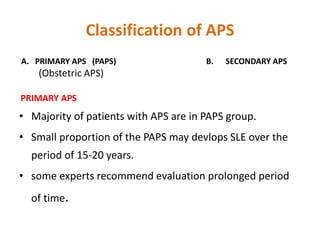
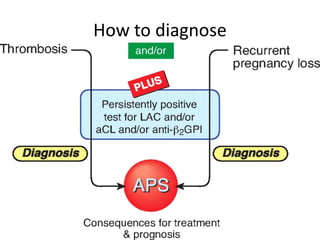
- APS was first described by Graham Hughes in 1983 and is characterized by arterial or venous thrombosis and/or pregnancy morbidity in the presence of antiphospholipid antibodies.
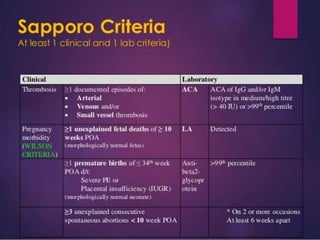
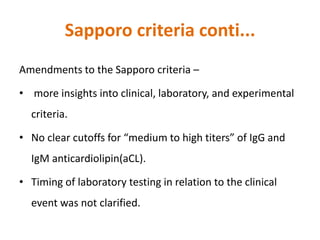
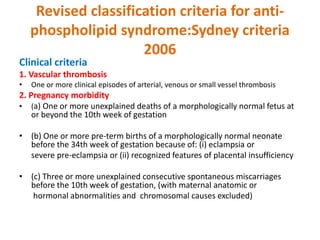
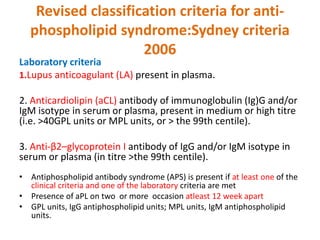
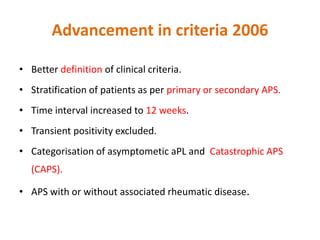
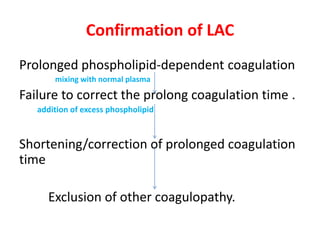
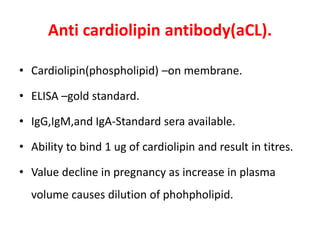
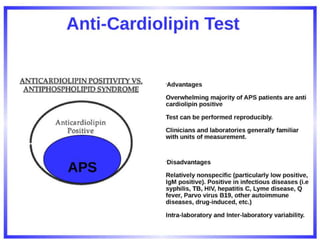
- International criteria were established in Sapporo in 1998 and revised in Sydney in 2006 to better define the clinical and laboratory criteria for diagnosing APS.
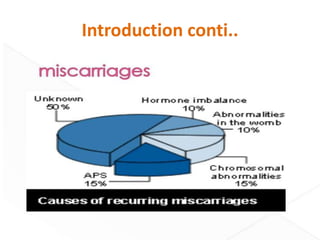
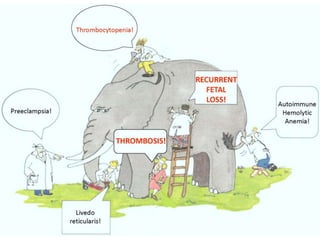
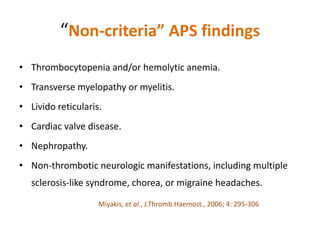
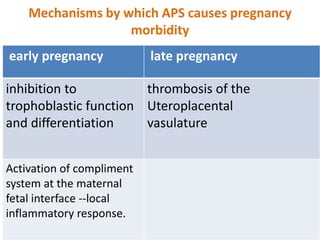
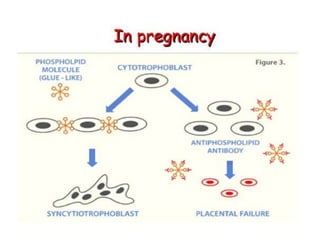
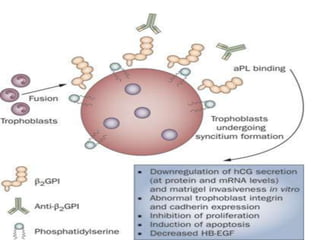
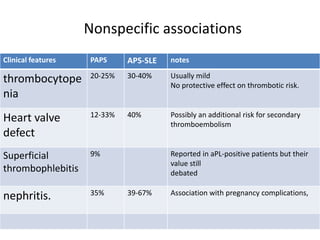
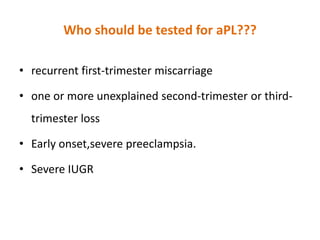
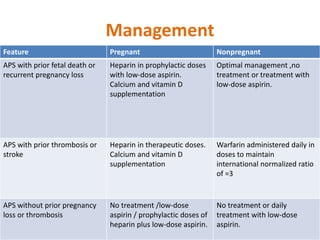
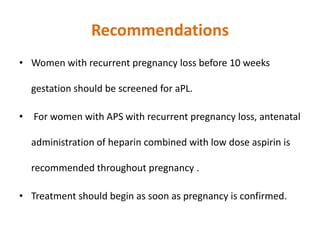
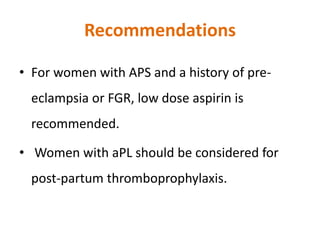
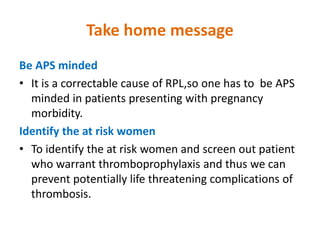
- APS can cause a variety of clinical complications including thrombosis, pregnancy loss, heart valve disease, and neurological symptoms. Recurrent pregnancy loss is a hallmark of obstetric APS.