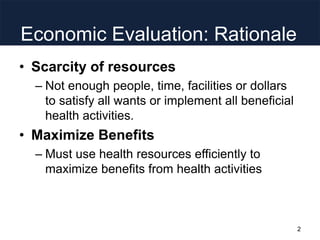
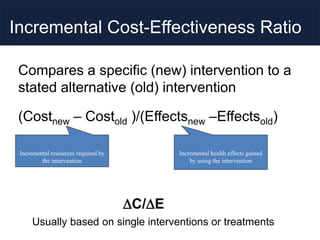
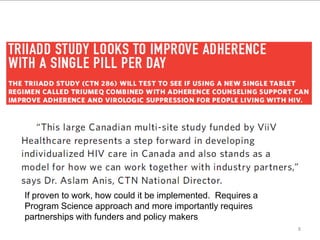
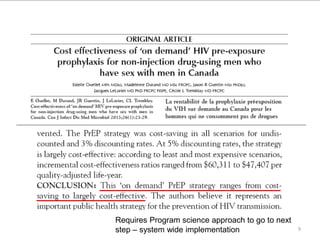
The document discusses the importance of economic evaluation and cost-effectiveness in program science, emphasizing the necessity of maximizing health resources in light of their scarcity. It highlights innovative approaches to HIV prevention and the application of complex systems modeling to improve healthcare logistics and decision-making. The conclusion stresses the potential for interdisciplinary collaboration in enhancing healthcare quality and system performance.