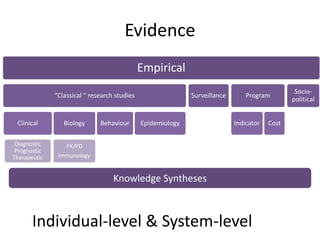
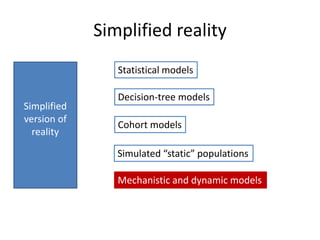
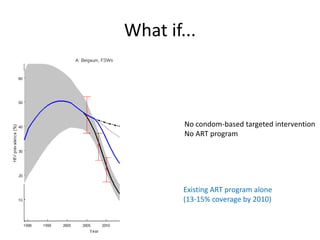
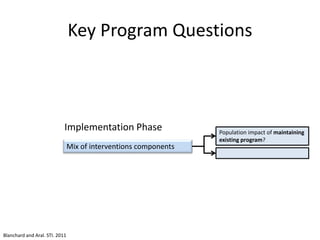
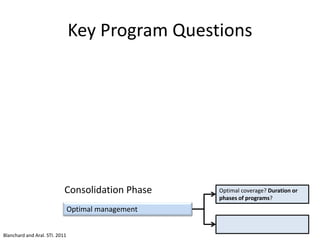
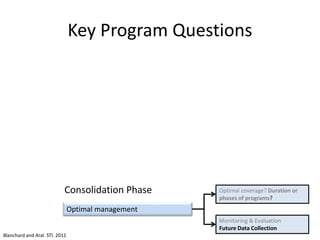
Mathematical models can help answer key questions in program science by examining disease transmission dynamics at a population level. Program science can also inform mathematical modeling by generating data to validate and refine models, and asking novel questions that require new modeling approaches. Both fields stand to benefit from stronger collaboration, with program science generating diverse data to feed into models, and models providing insights into optimal intervention strategies under uncertainty.