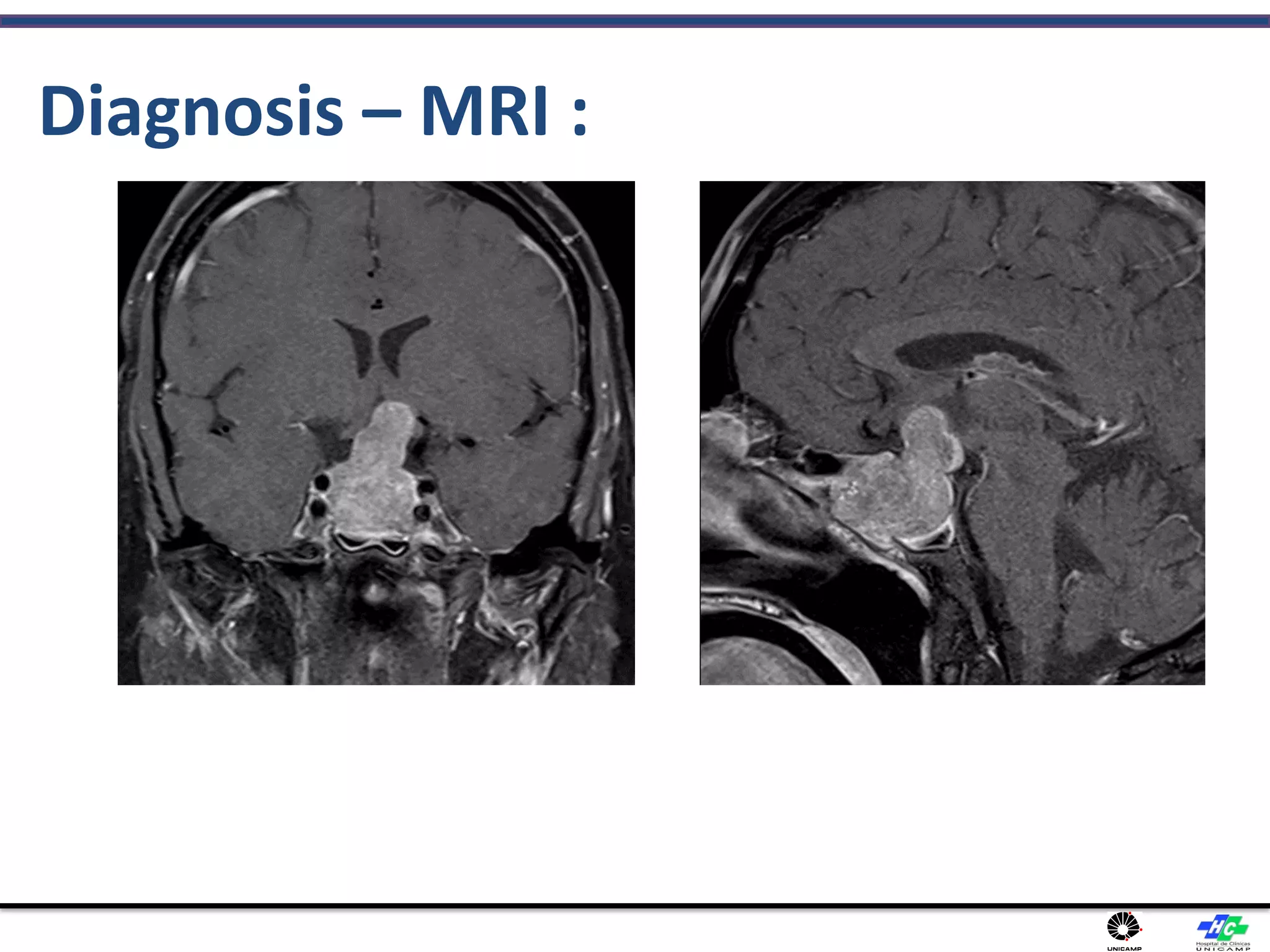
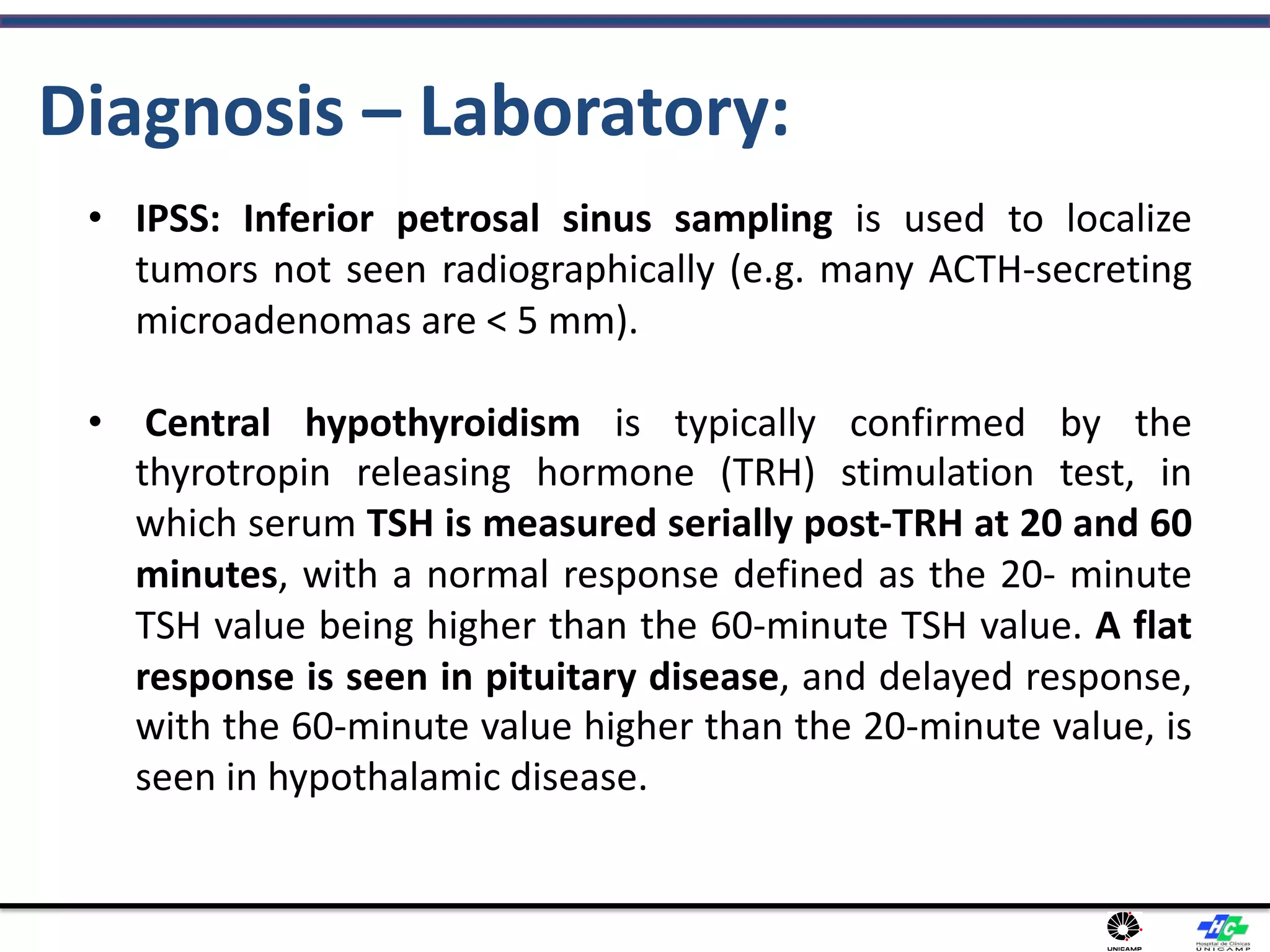
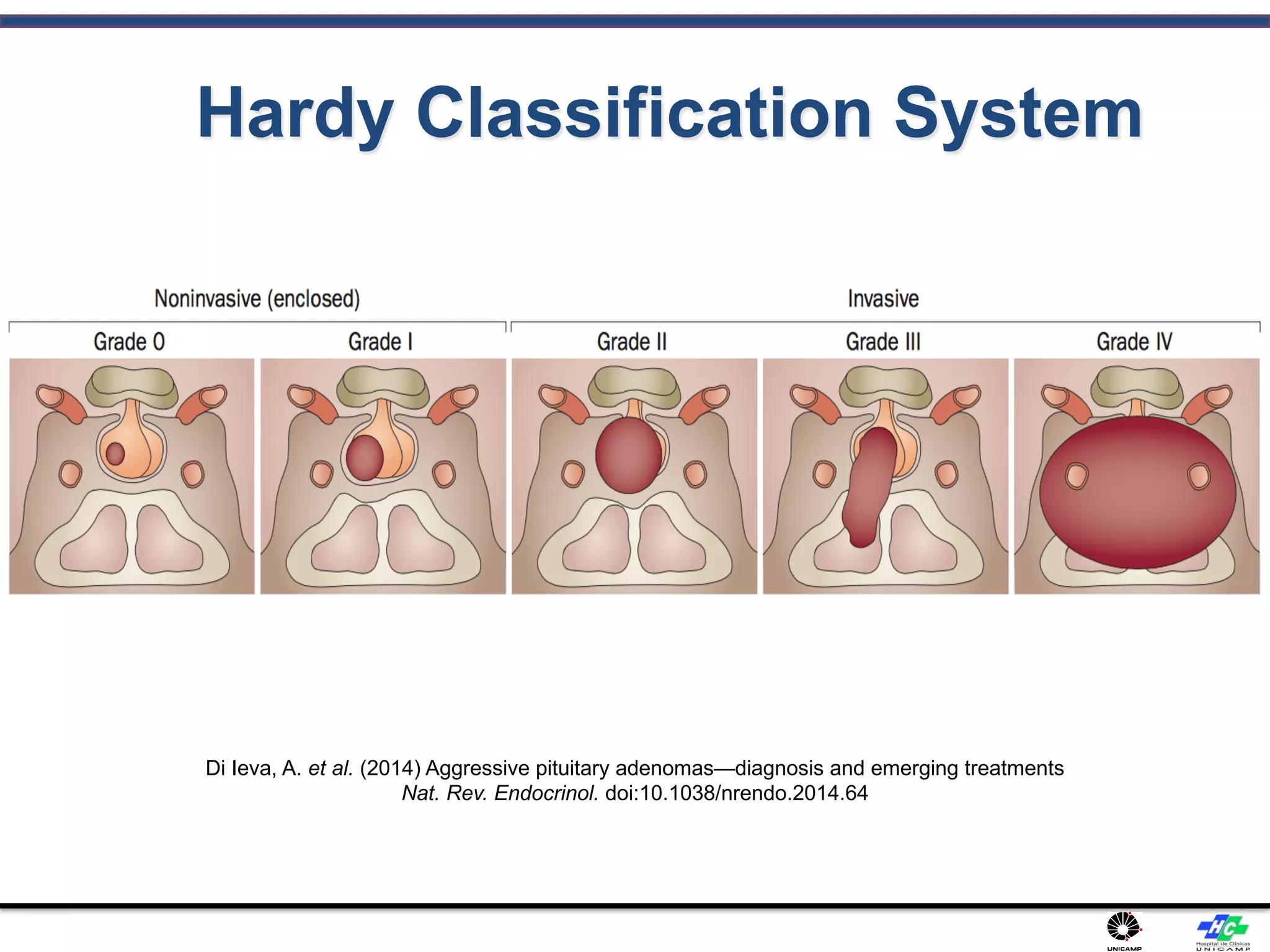
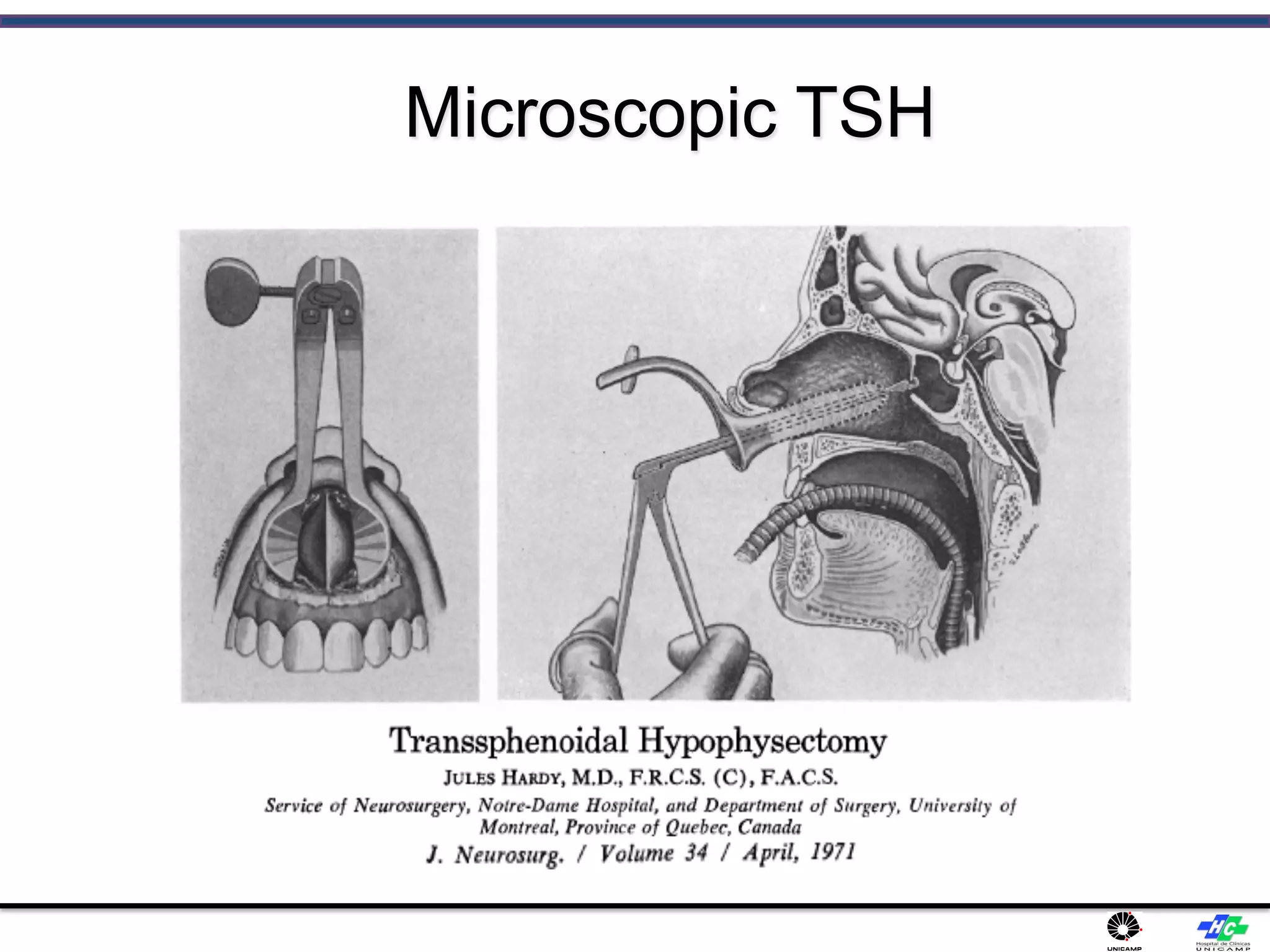
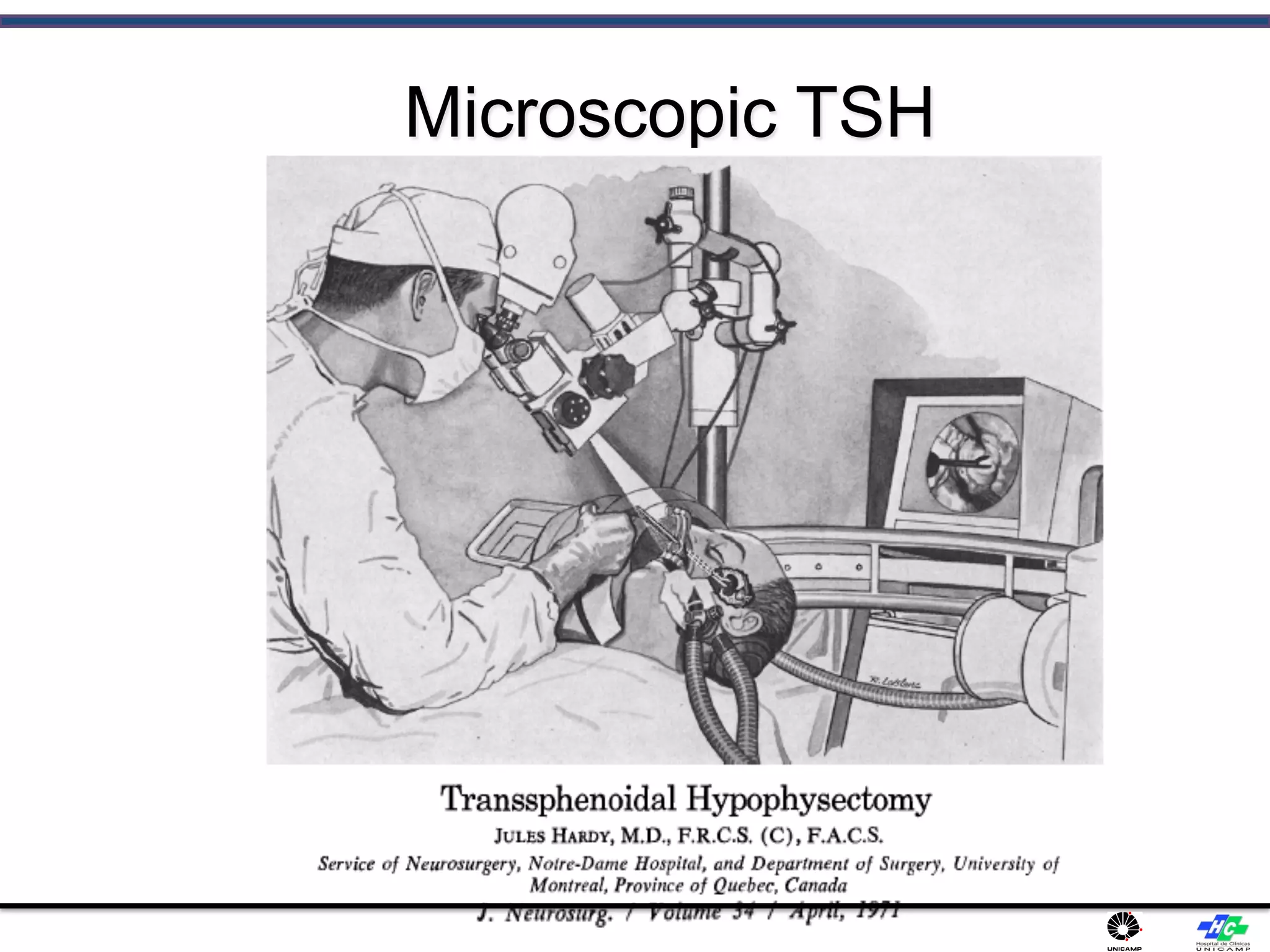
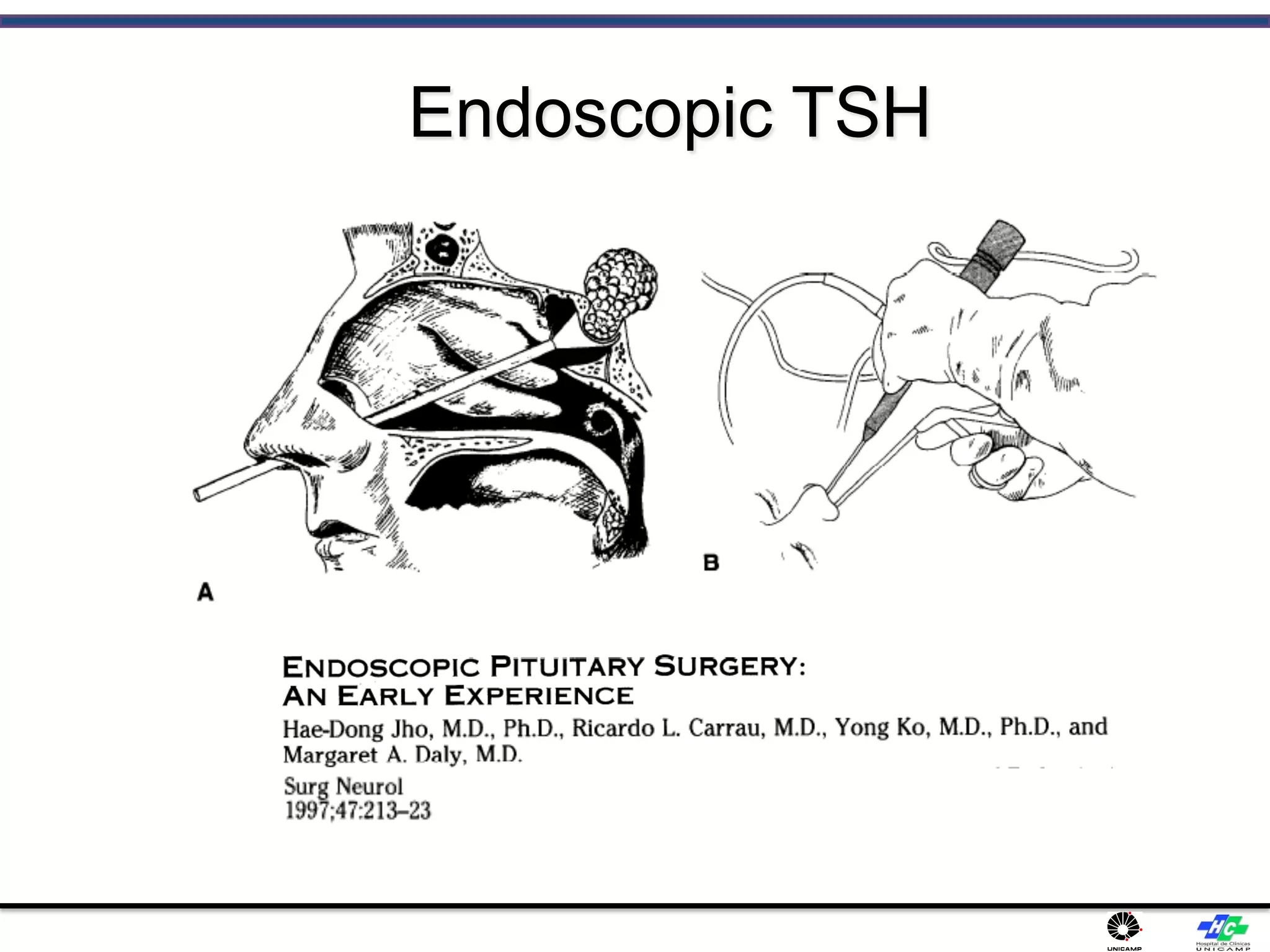
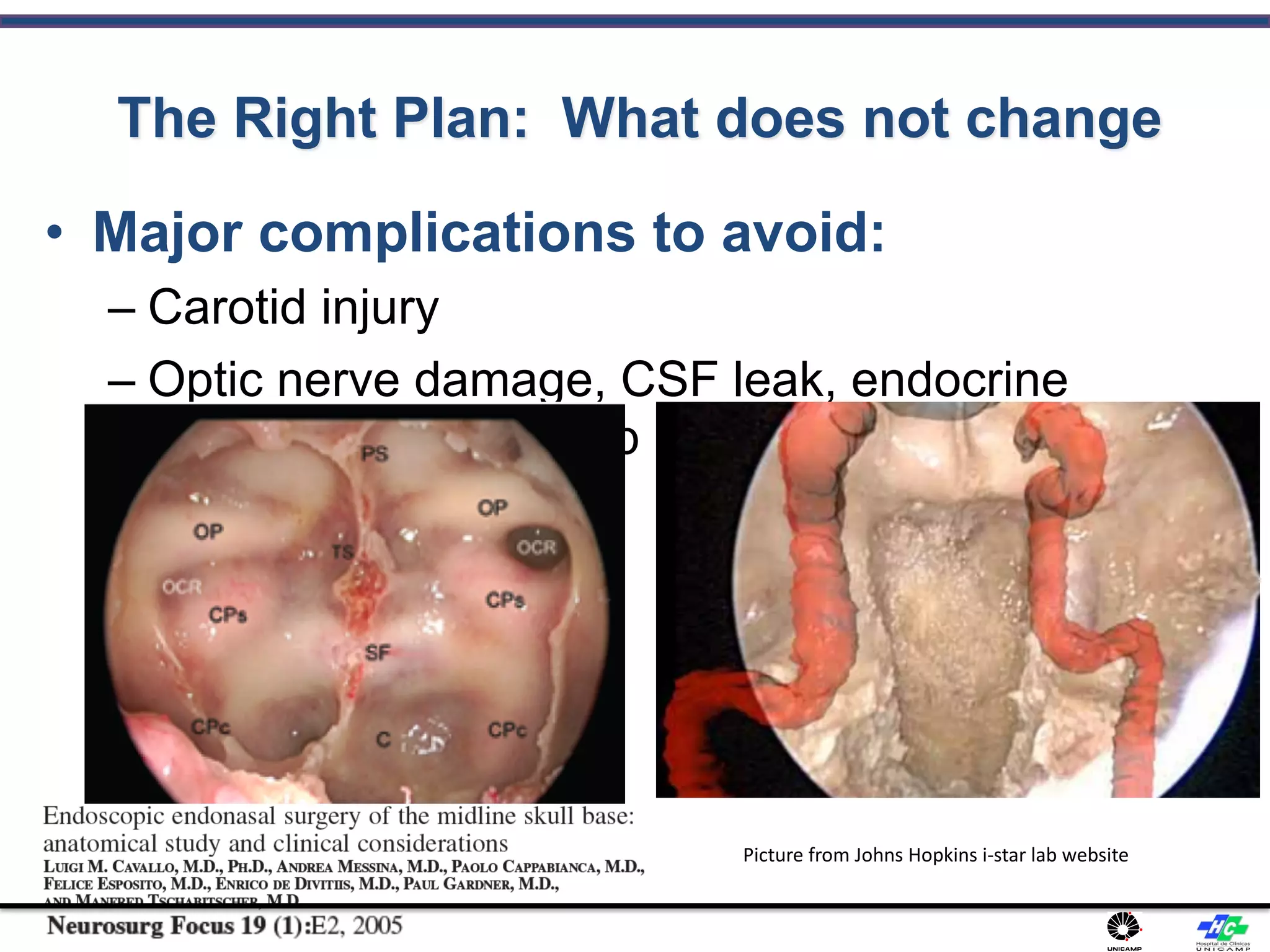
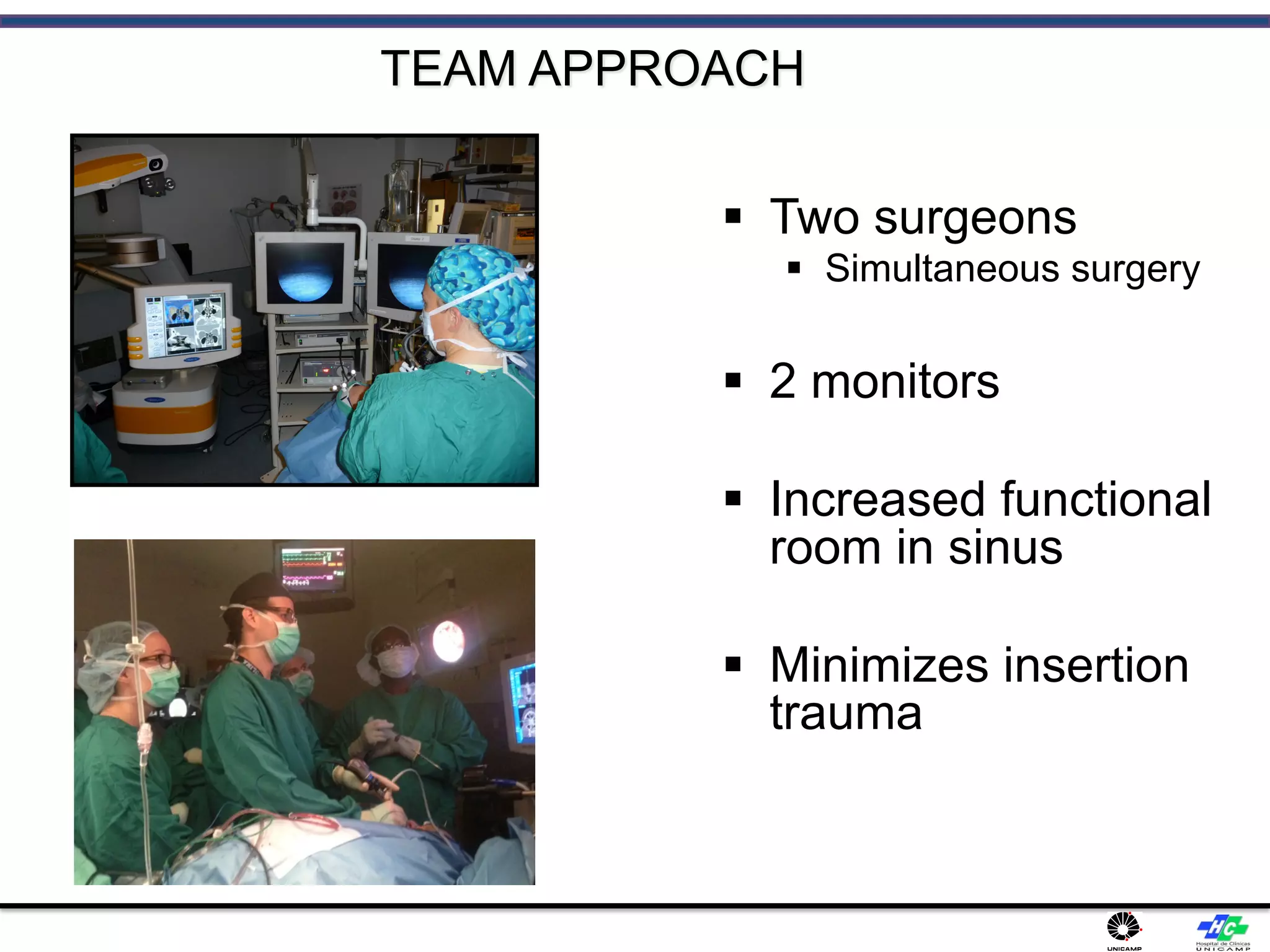
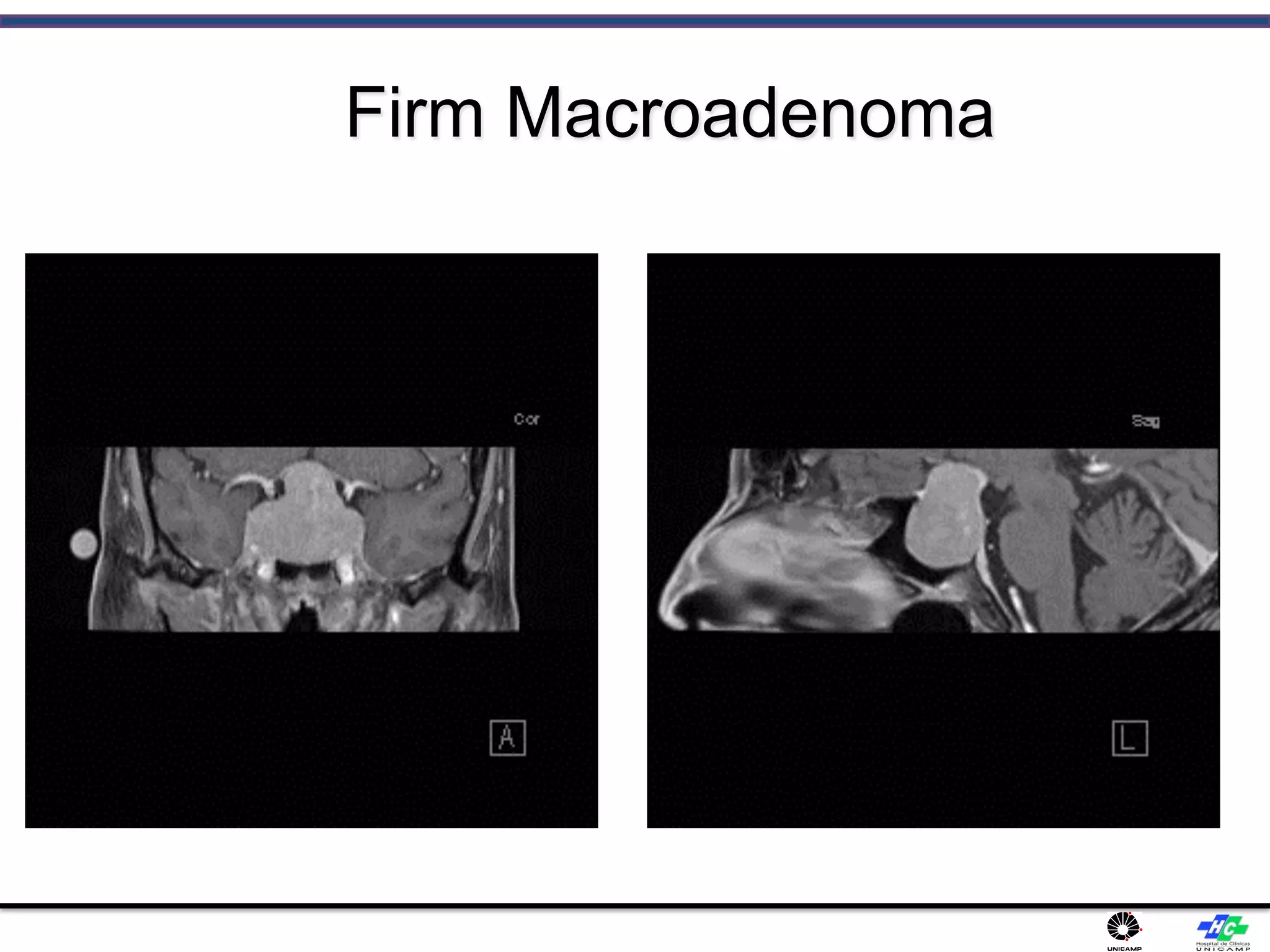
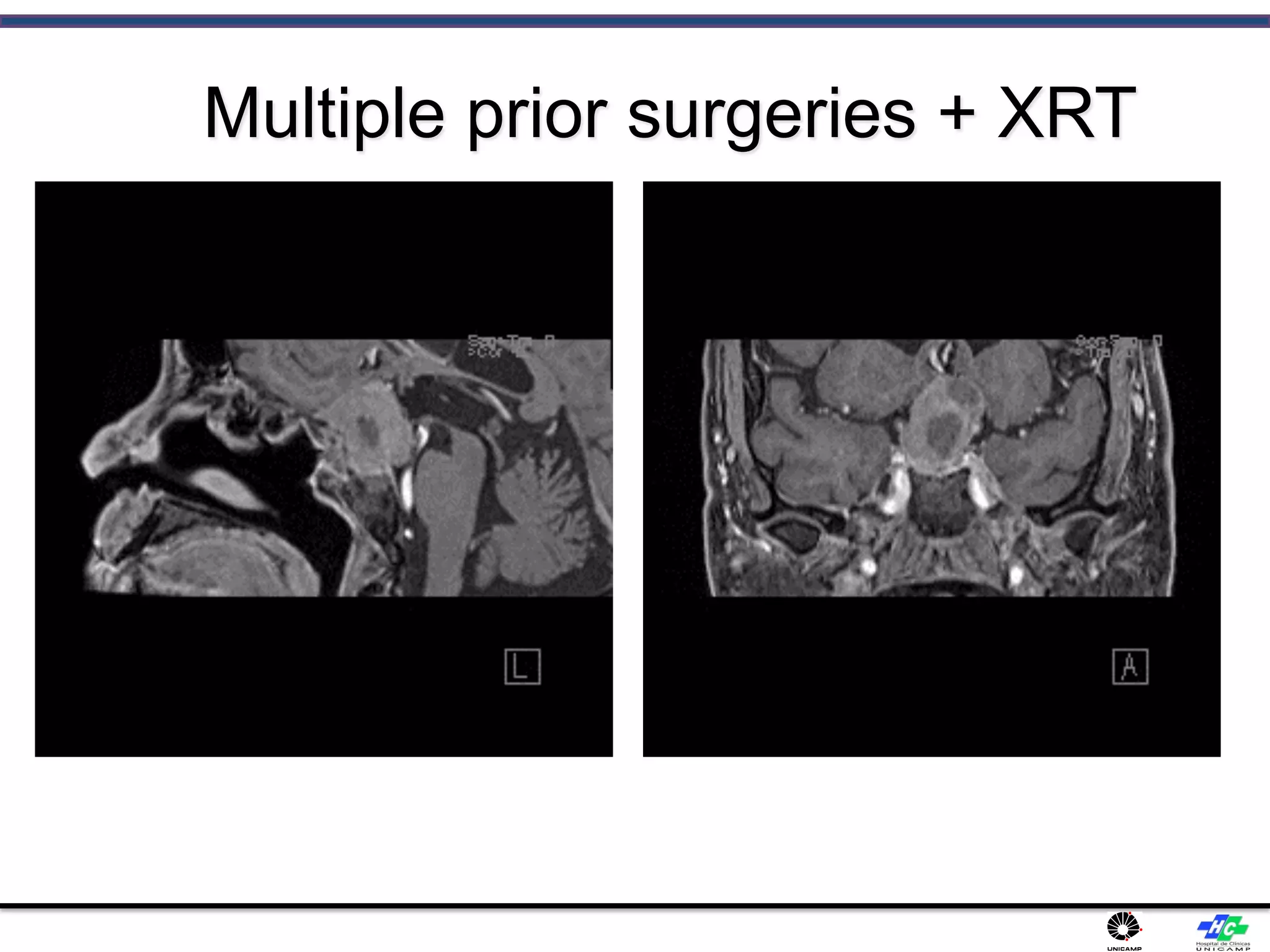
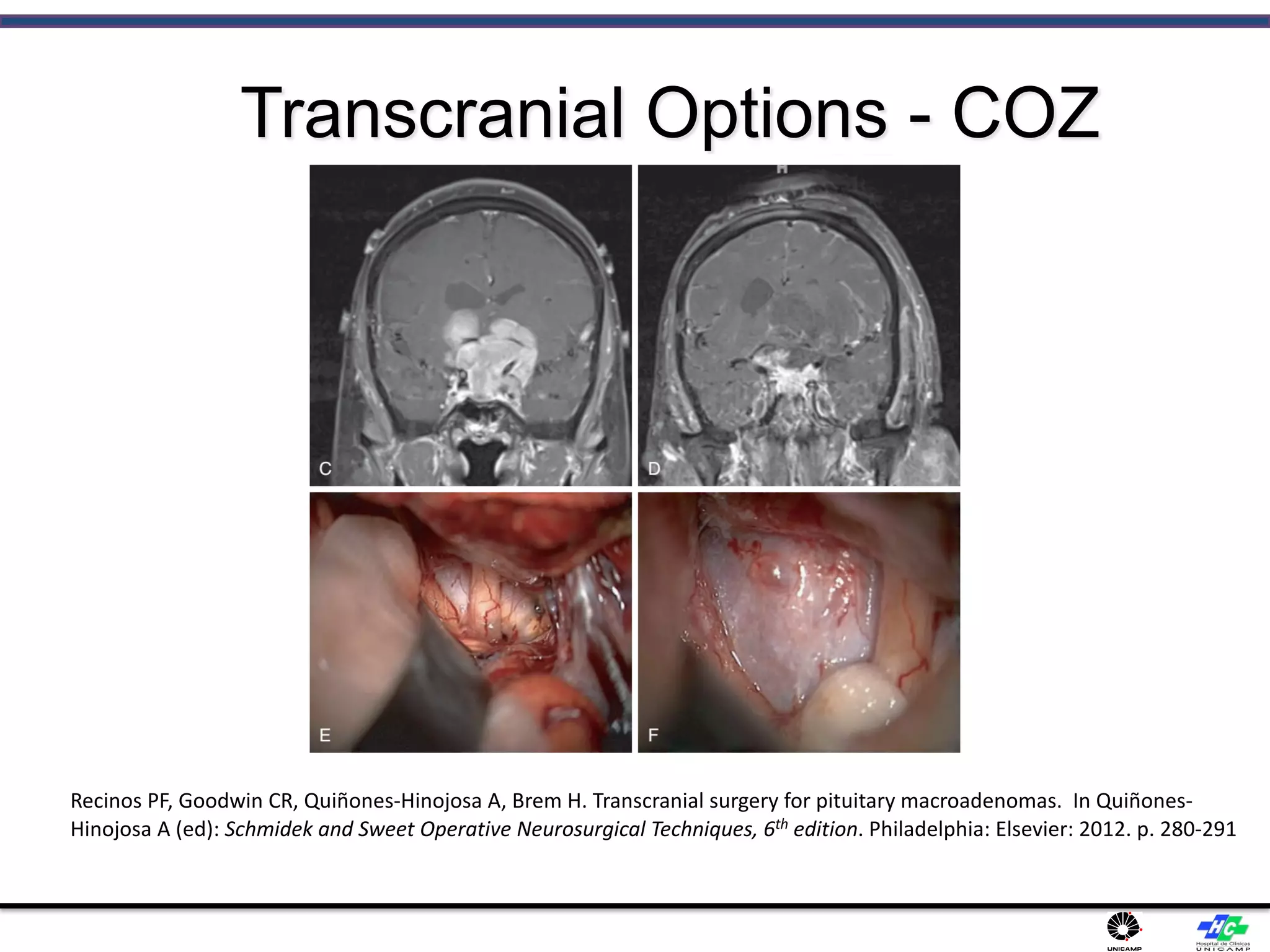
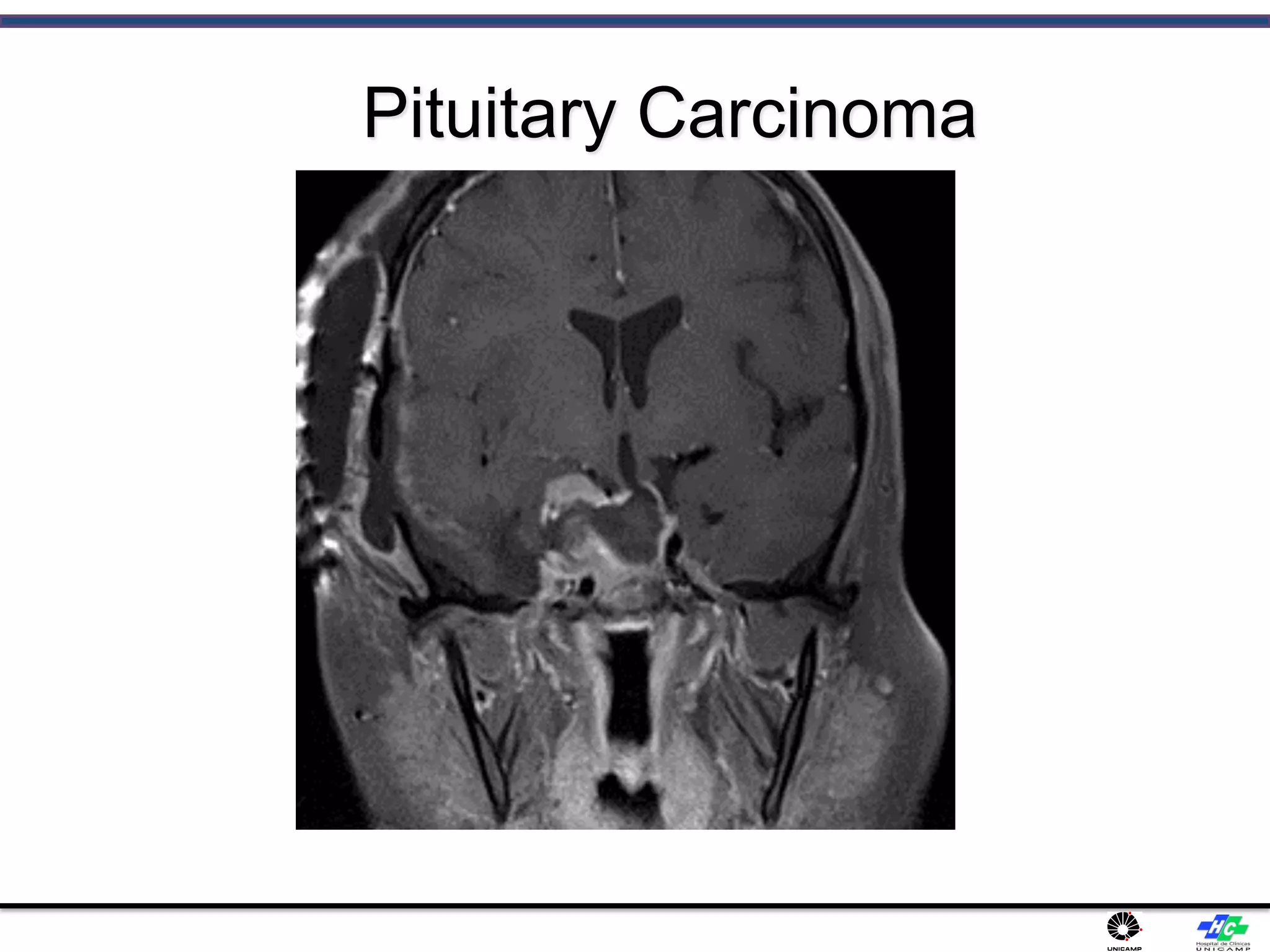
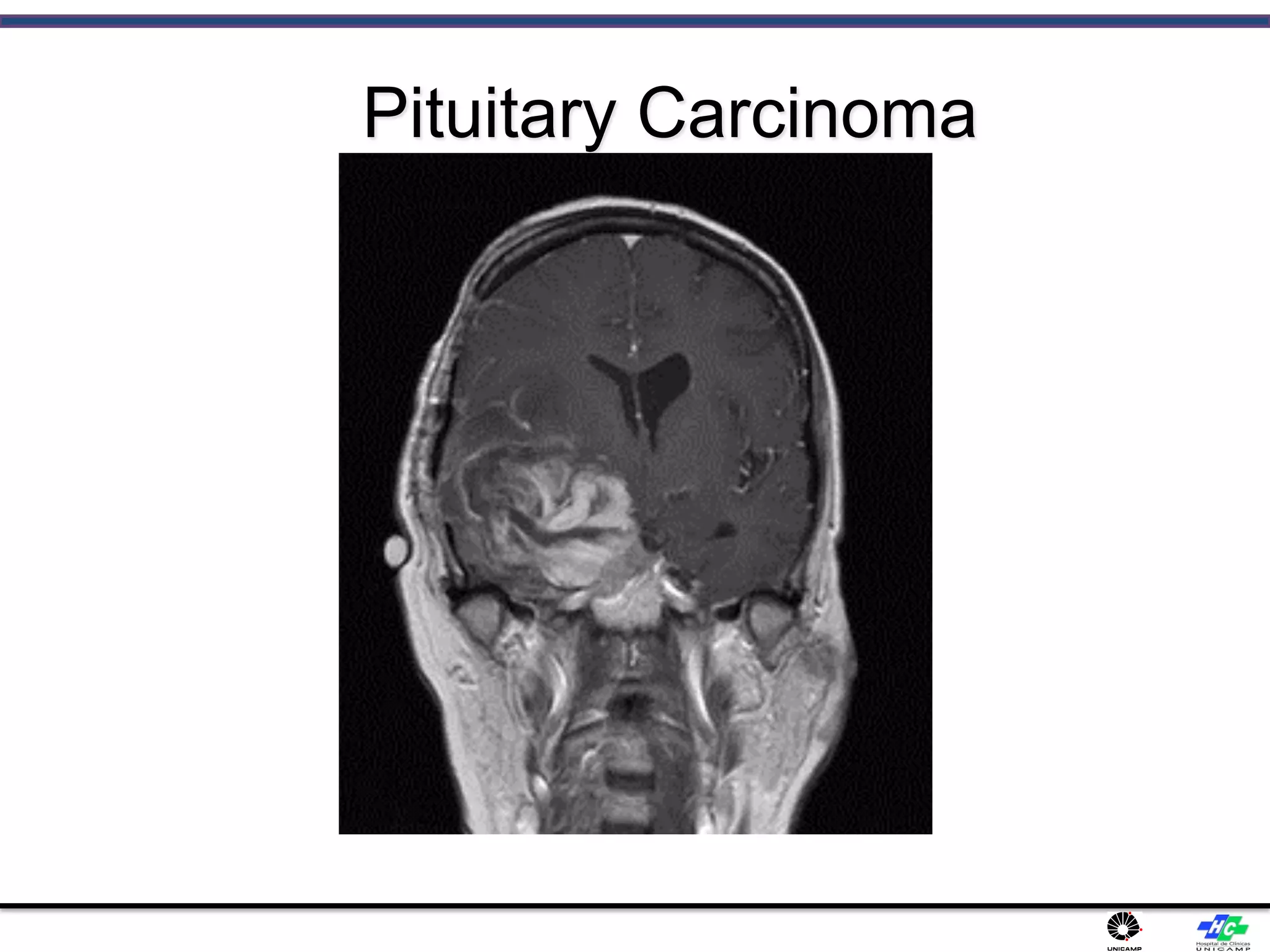
The document provides a comprehensive overview of pituitary adenomas, including their epidemiology, clinical features, and diagnostic methods. It discusses tumor development, hormonal functions, and complications such as headaches and visual disturbances. The manuscript emphasizes contemporary surgical management approaches, particularly the expanded endoscopic endonasal techniques, highlighting their benefits in treating aggressive cases and the importance of a multidisciplinary approach.