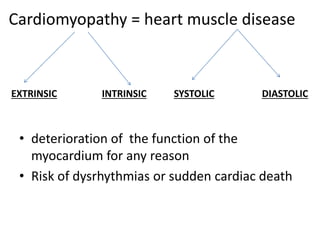
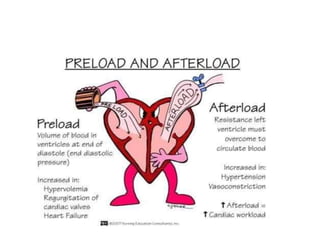
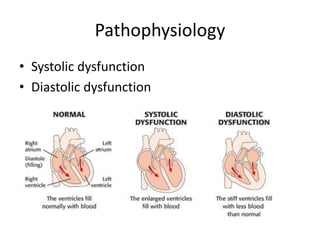
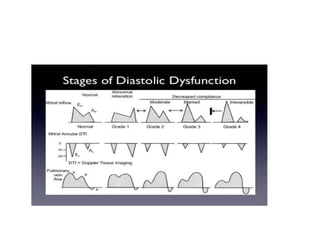
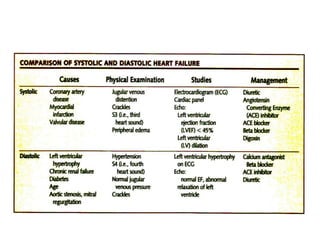
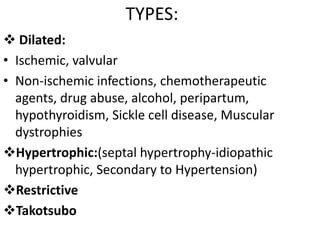
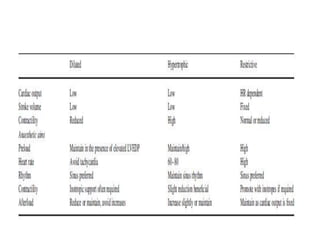
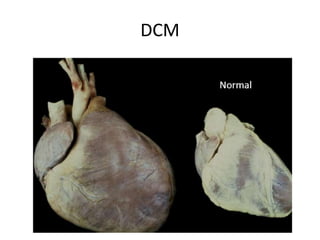
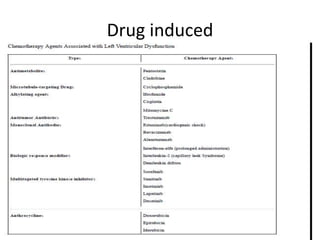
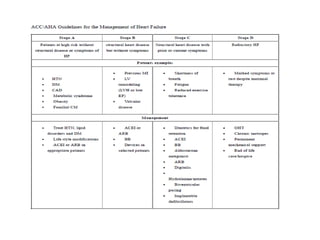
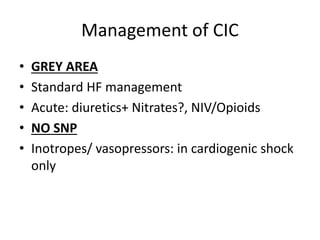
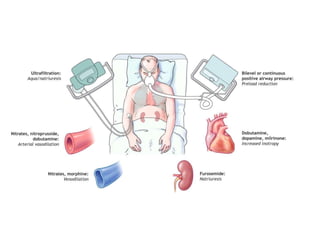
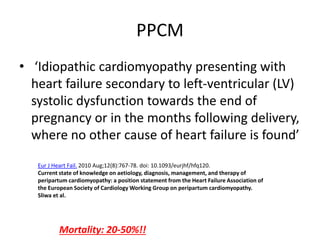
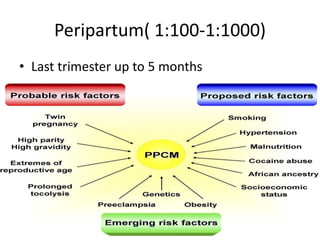
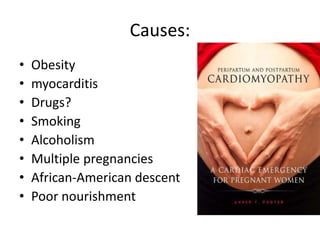
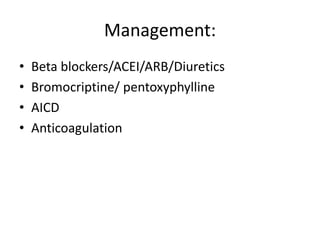
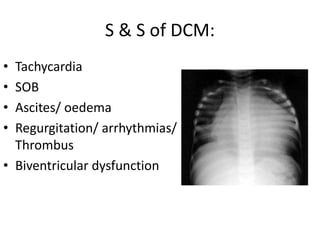
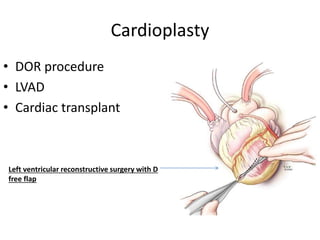
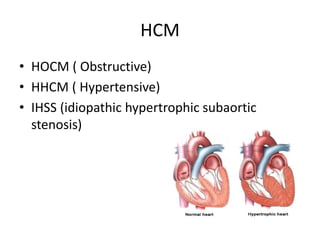
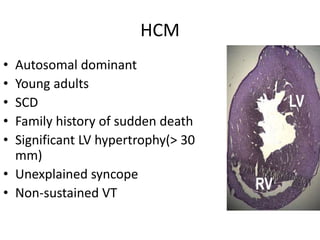
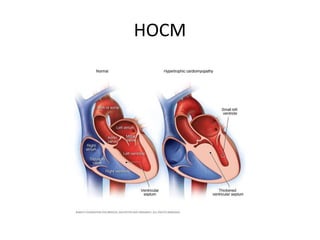
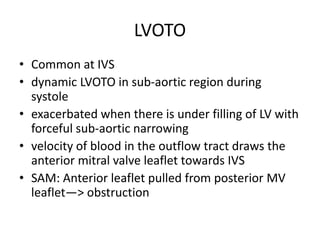
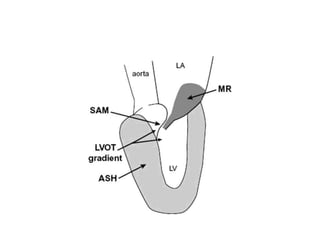
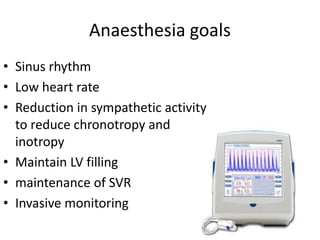
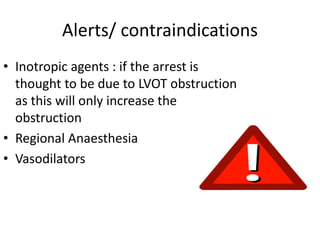
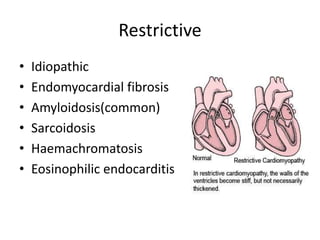
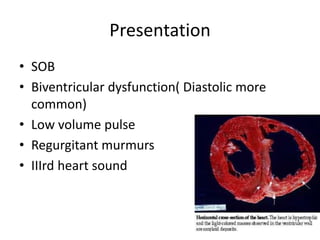
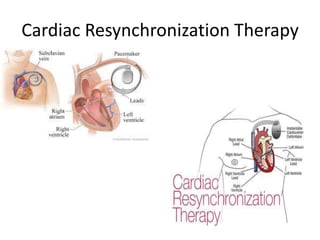
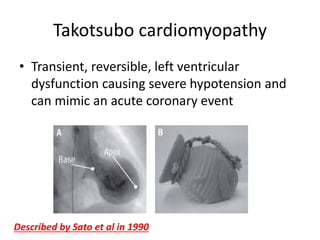
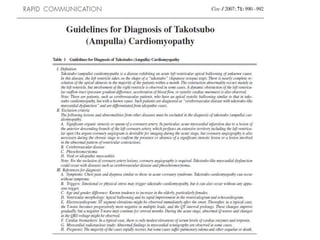
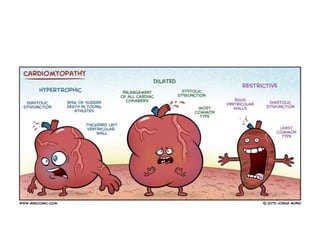
The document covers various aspects of cardiomyopathy and its management in the context of anesthesia, including types such as dilated, hypertrophic, and restrictive cardiomyopathy. It outlines the pathophysiology, causes, and treatment strategies, emphasizing the importance of careful monitoring and management of patients with heart function issues during anesthesia. Additionally, it addresses specific considerations for anesthetic approaches, including the avoidance of certain agents and the maintenance of hemodynamic stability.