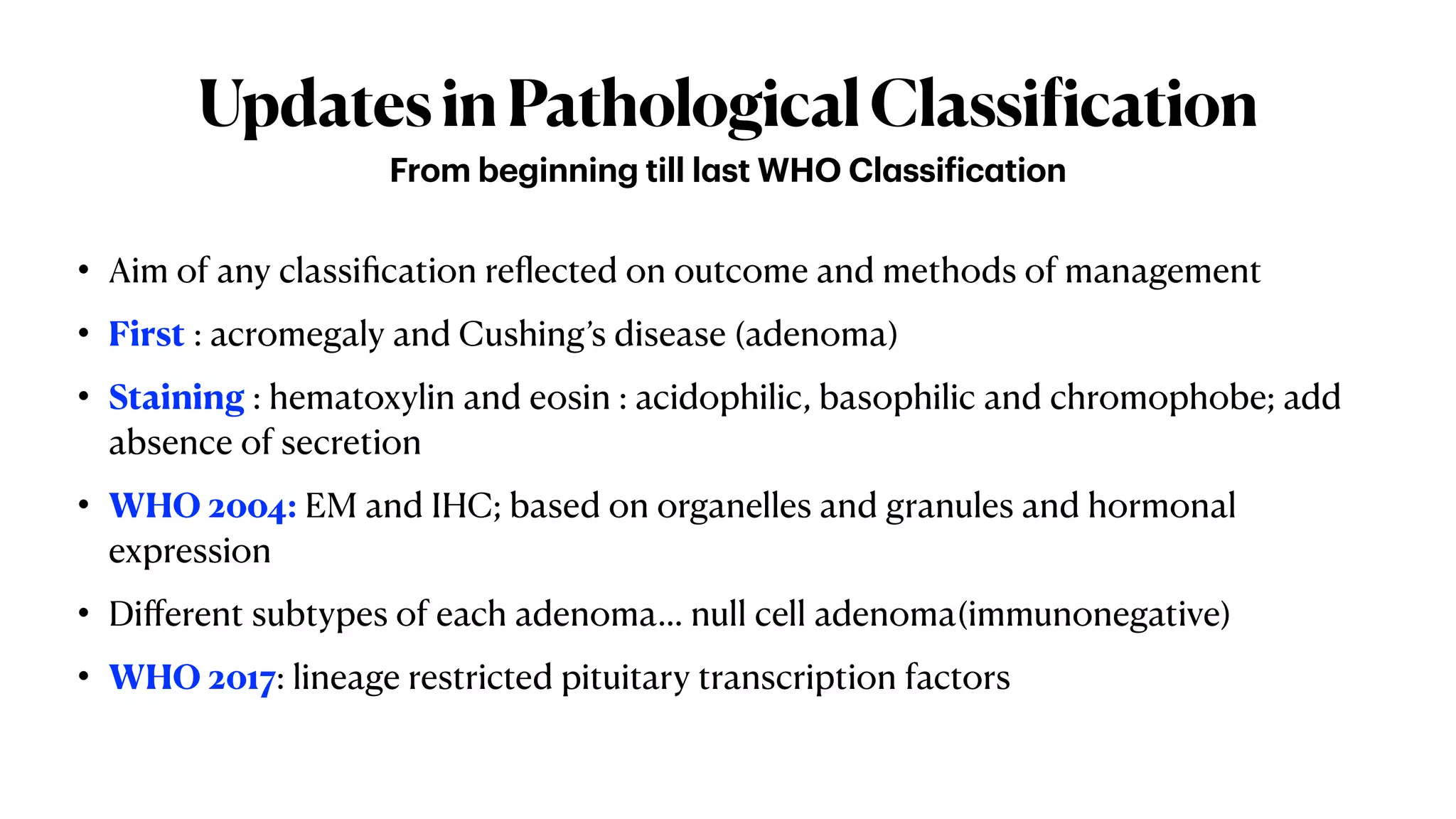
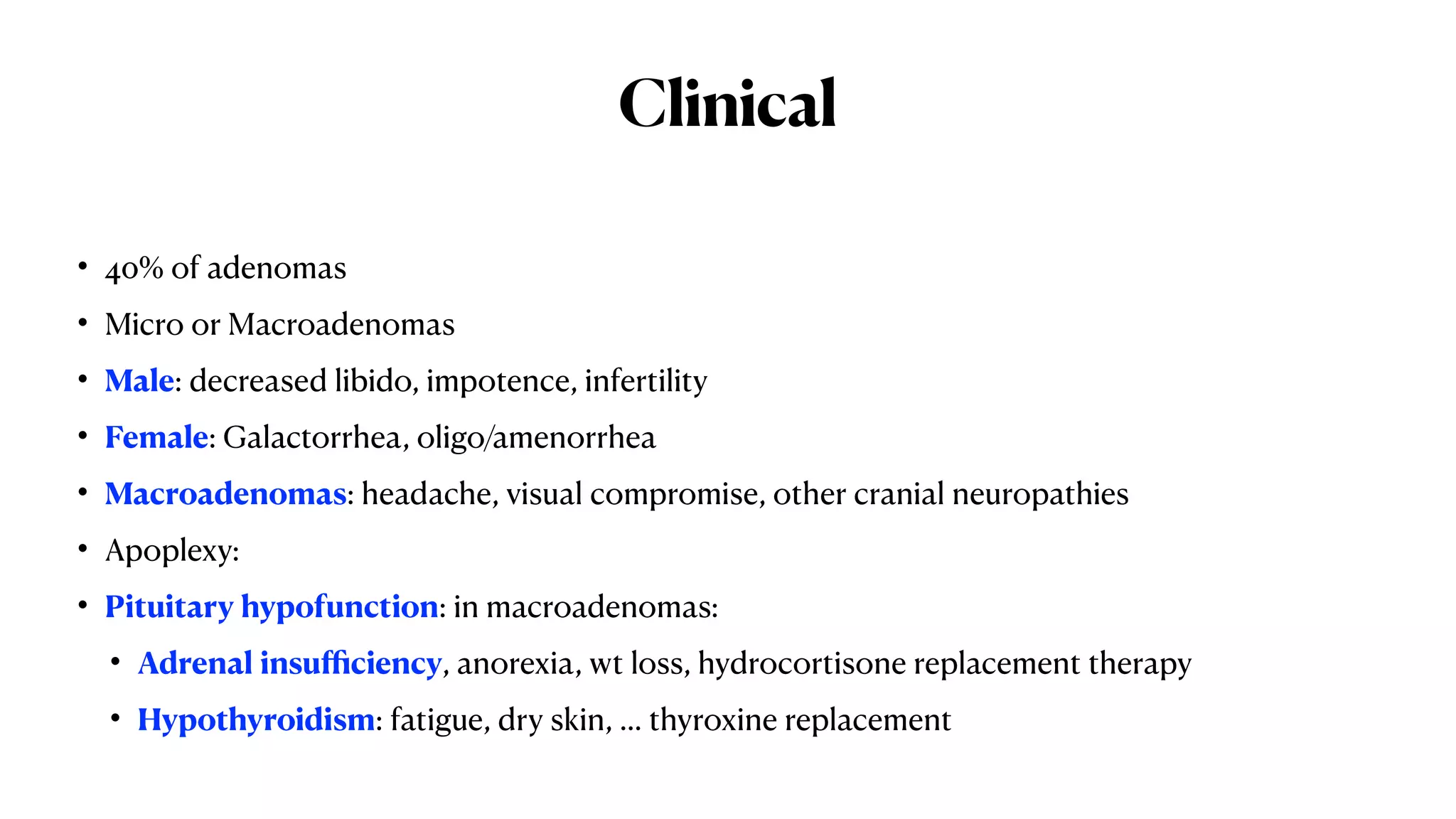
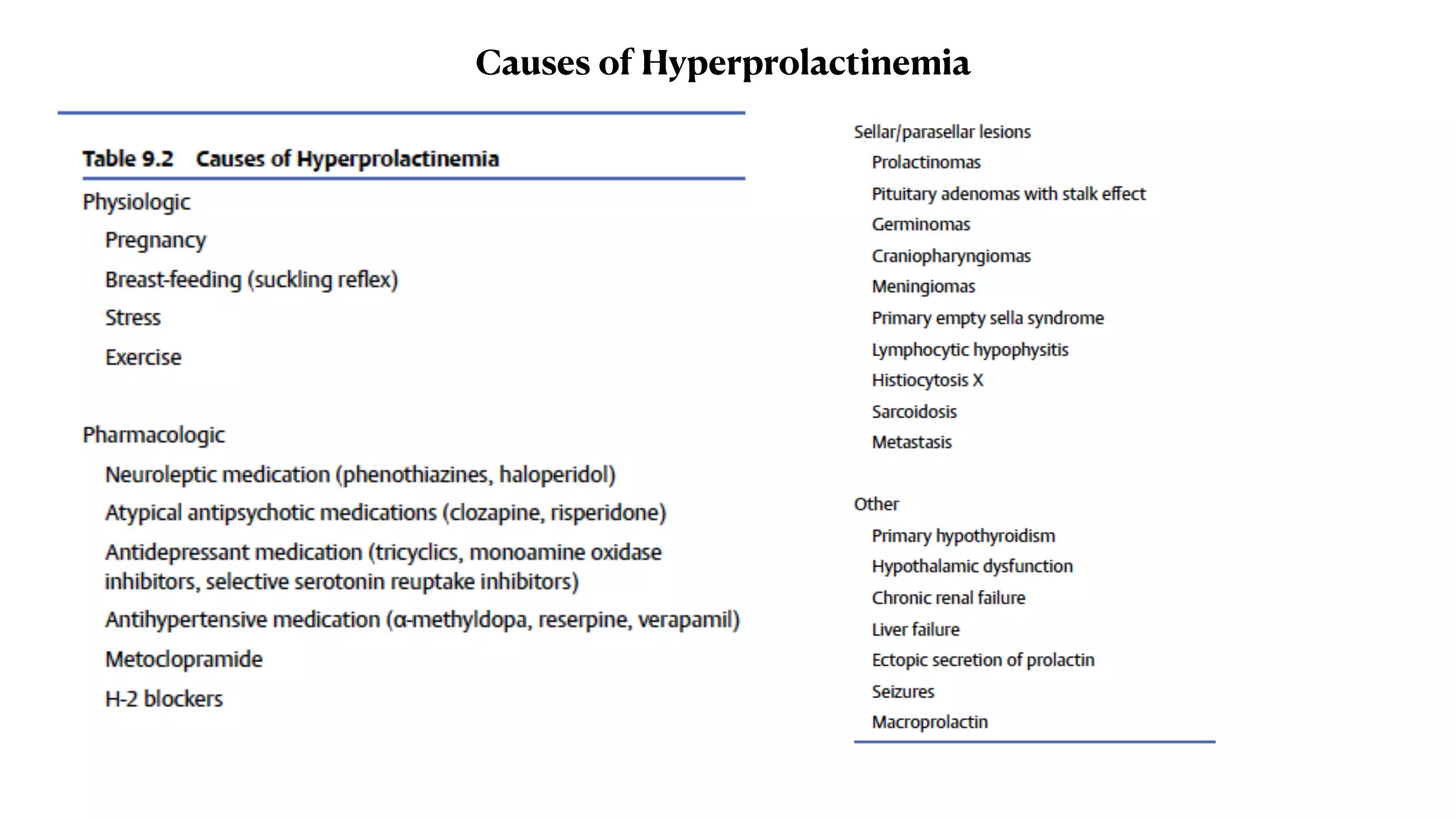
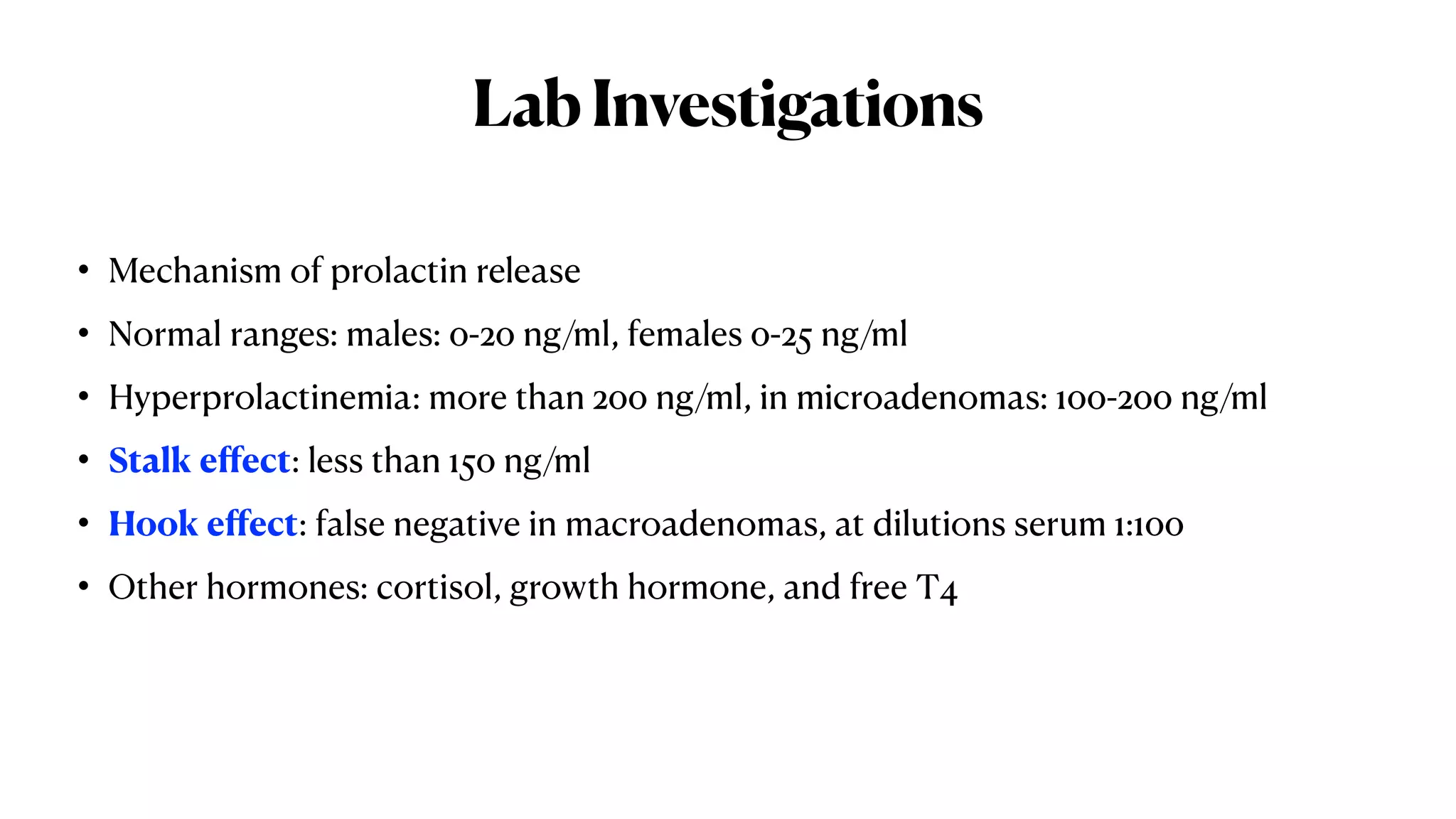
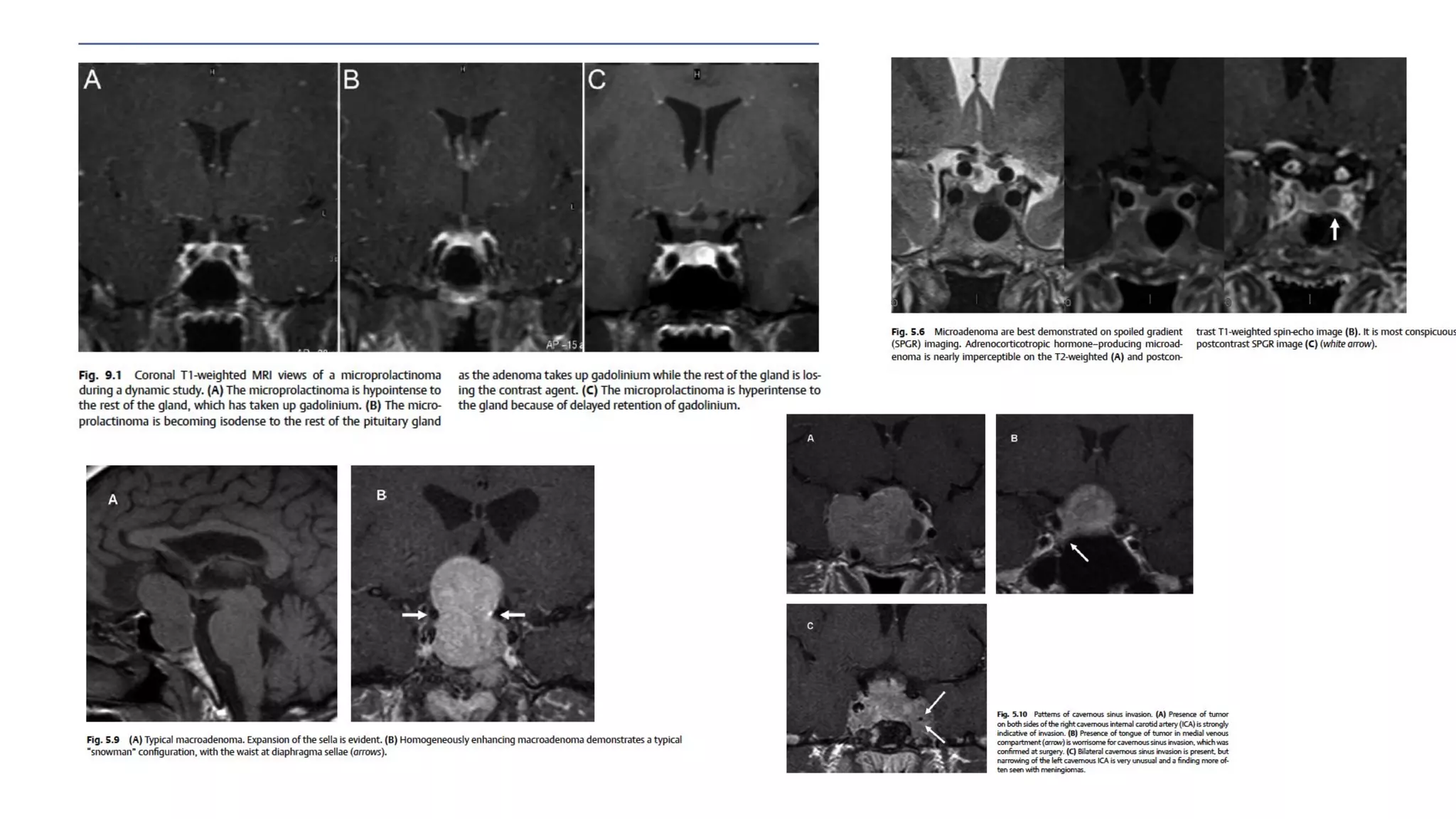
This document summarizes a webinar on prolactinomas and their management. It discusses the anatomy and histology of the pituitary gland and pathological subtypes of prolactinomas according to the new WHO classification. Clinical presentations, investigations including lab tests, visual and radiological assessments are outlined. Medical management using dopamine agonists and surgical management via different approaches are described. Complications like apoplexy and management of invasive prolactinomas are also summarized. The conclusion reiterates that prolactinomas are the second most common pituitary adenomas and various treatment approaches are available depending on the subtype and presentation of individual cases.