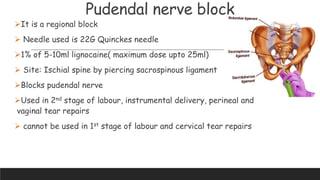
This document discusses different types of anesthesia used in obstetrics. It begins with definitions of anesthesia and a brief history. The main types covered are spinal, epidural, continuous spinal and general anesthesia. Spinal anesthesia is preferred due to rapid onset, awake patient during birth, and decreased risk of complications. Epidural is commonly used for labor analgesia. Techniques, advantages, and complications are described for each type. The document also discusses regional blocks like paracervical and pudendal nerve blocks.