This document provides an overview of anaemia, including its definition, causes, risk factors, pathophysiology, classification, clinical manifestations, diagnostic tests, medical management, and nursing care. Key points include:
- Anaemia is a reduction in red blood cells, haemoglobin, or hematocrit, causing tissue hypoxia. It can be caused by blood loss, decreased red blood cell production, or increased red blood cell destruction.
- Common causes include iron, vitamin B12, or folate deficiencies, blood loss, bone marrow disorders, and haemolytic disorders.
- Signs and symptoms vary depending on severity but can include pallor, fatigue, weakness, and shortness of breath.
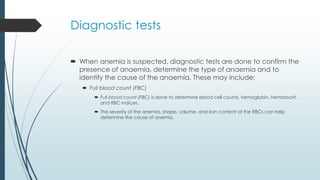
- Diagnostic











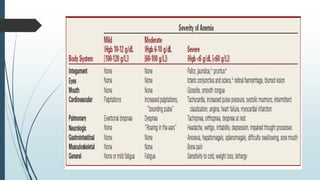
![Clinical Manifestations
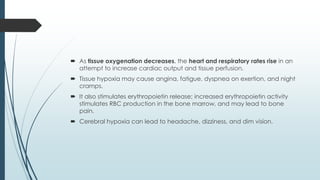
Are caused by the body’s response to tissue hypoxia.
Specific manifestations vary depending on the rate at which the anemia
has evolved, its severity, and any coexisting disease.
Mild states of anemia (Hgb 10 to 12 g/dL [100 to 120 g/L]) may exist without
causing symptoms.
If symptoms develop, it is because the patient has an underlying disease or
is experiencing a compensatory response to heavy exercise.](https://image.slidesharecdn.com/anaemia-220803154940-92f1f733/85/ANAEMIA-pdf-21-320.jpg)
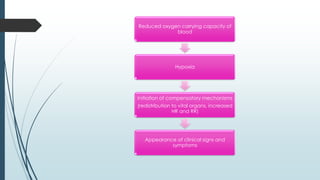
![ Symptoms include palpitations, dyspnea, and mild fatigue.
In moderate anemia (Hgb 6 to 10 g/dL [60 to 100 g/L]) the
cardiopulmonary symptoms are increased.
The patient may experience them while resting, as well as with activity.
In severe anemia (Hgb less than 6 g/dL [60 g/L]) the patient has many
clinical manifestations involving multiple body systems](https://image.slidesharecdn.com/anaemia-220803154940-92f1f733/85/ANAEMIA-pdf-22-320.jpg)