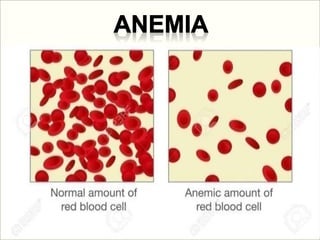
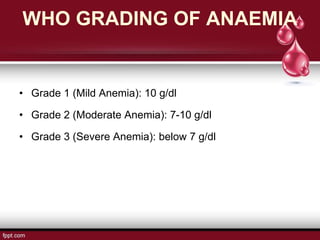
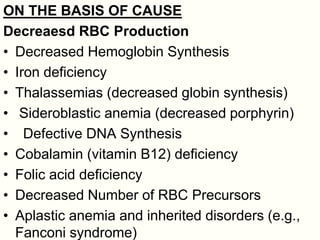
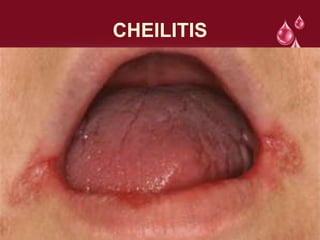
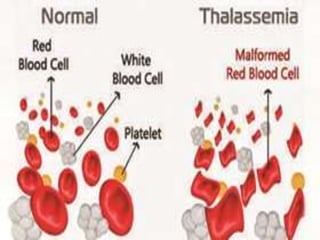
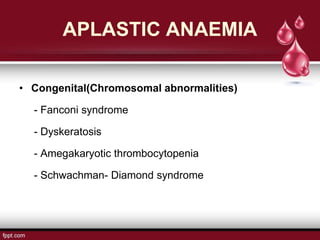
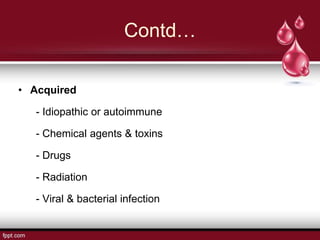
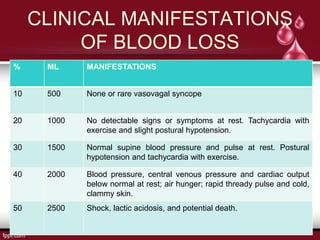
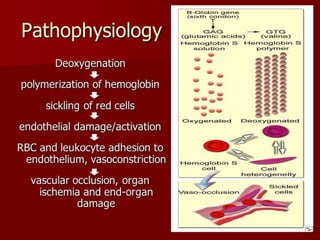
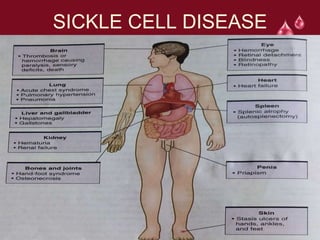
The document discusses anemia as a condition characterized by low hemoglobin levels due to nutrient deficiencies, classifying it into grades and outlining causes such as decreased red blood cell production, blood loss, and increased destruction. It further details various types of anemia, including thalassemia and aplastic anemia, with their respective clinical manifestations and complications. Additionally, it highlights specific conditions linked to anemia and their effects on the body.