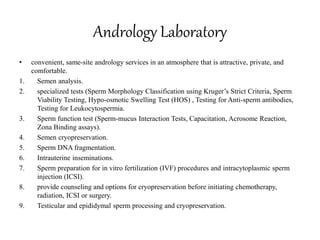
The document provides information about andrology laboratory services for male infertility evaluation and treatment. It discusses:
- Tests offered including semen analysis, specialized tests of sperm function and morphology, sperm processing for infertility treatments, and cryopreservation.
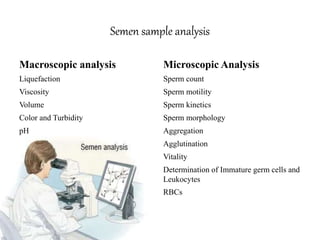
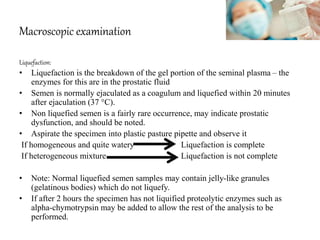
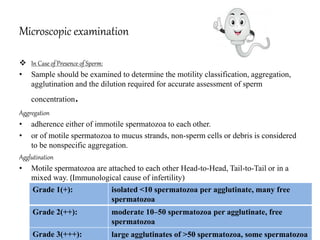
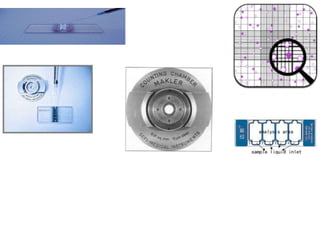
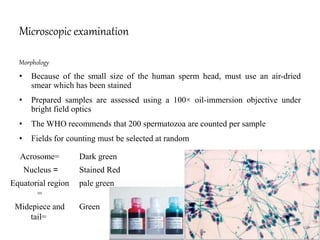
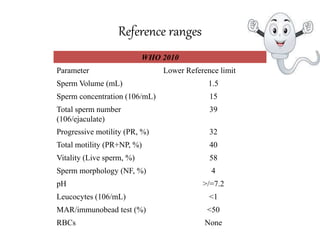
- Procedures for semen sample collection, transport, and analysis following WHO standards, including macroscopic examination of volume, pH, and microscopic examination of motility, concentration, vitality, and morphology.
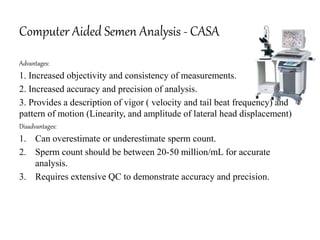
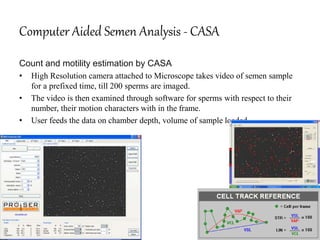
- Uses of semen analysis to diagnose infertility issues, identify treatment options, and assess effectiveness of treatments like vasectomy reversal. Computer-assisted semen analysis is also discussed.