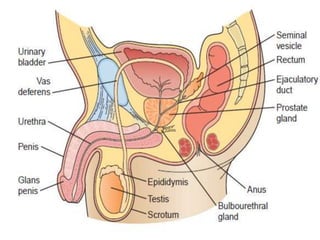
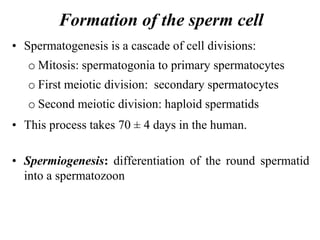
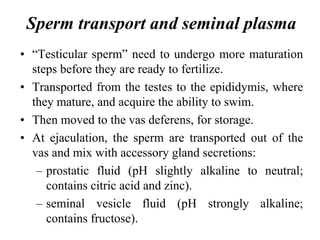
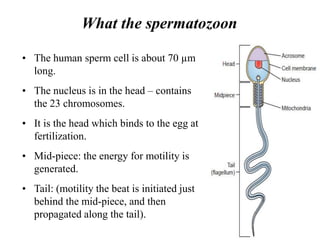
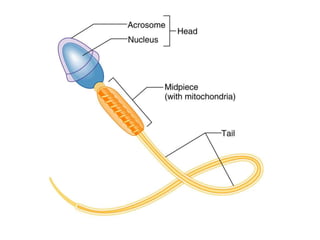
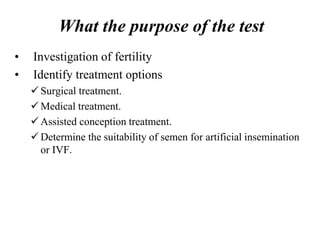
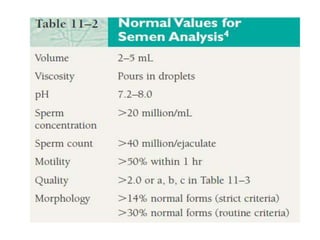
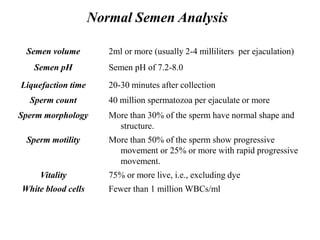
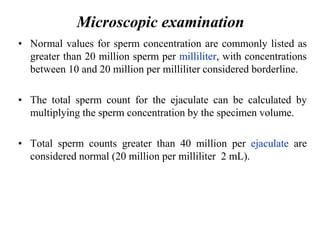
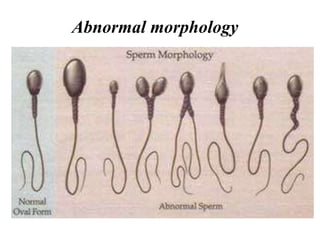
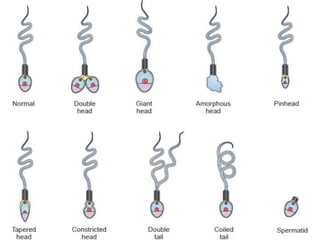
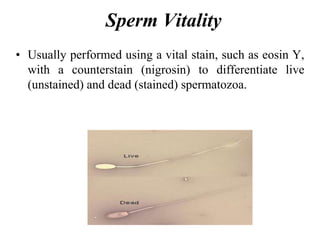
A semen analysis measures the amount and quality of semen and sperm to determine fertility. It analyzes semen volume, pH, sperm count, motility, morphology, and vitality. Sperm are produced in the testes and transported through the seminal vesicles and prostate to provide nutrients and protection. A semen analysis is an important first test for infertility, identifying potential issues affecting over 1/3 of couples unable to conceive.