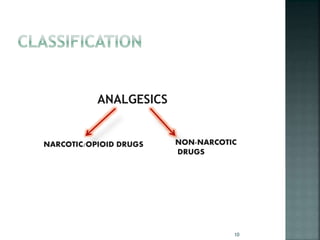
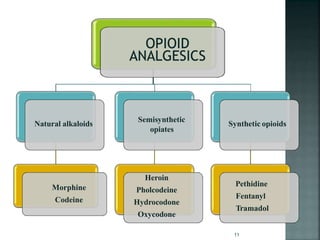
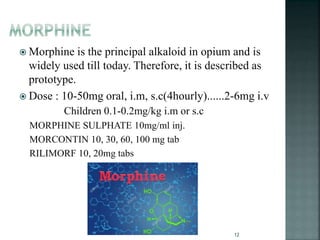
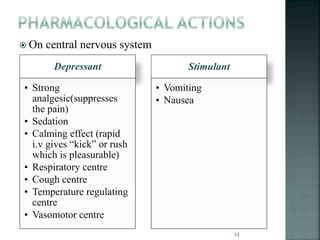
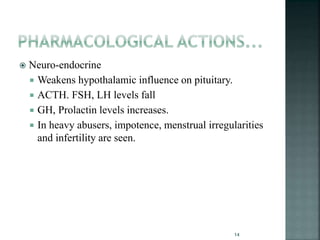
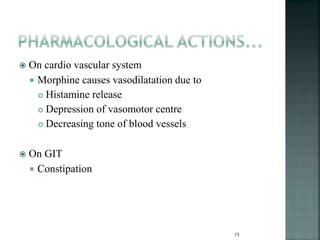
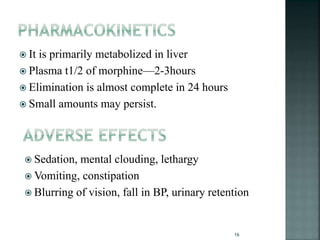
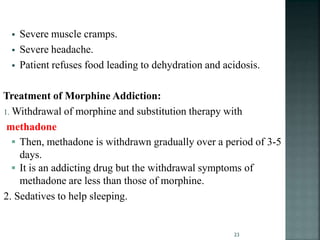
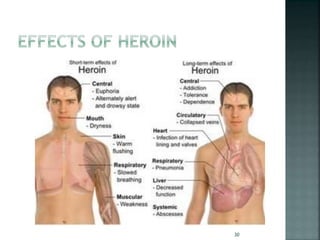
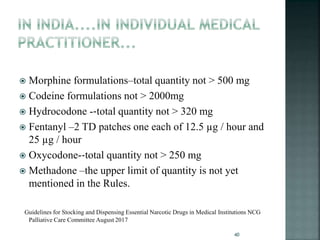
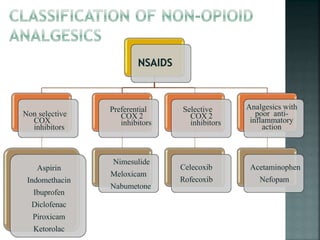
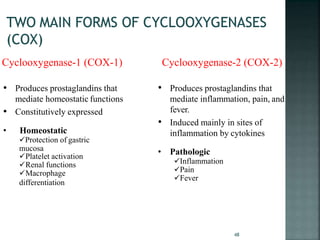
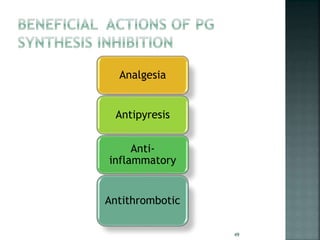
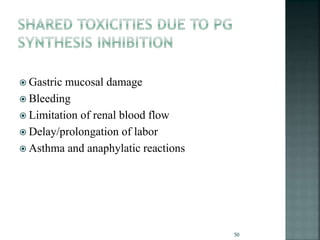
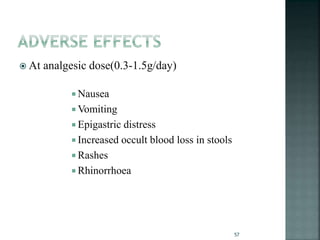
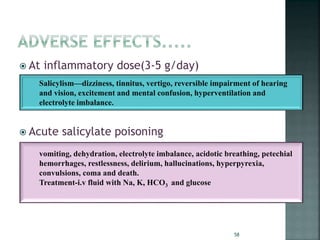
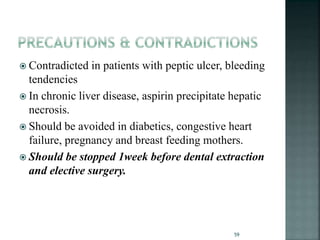
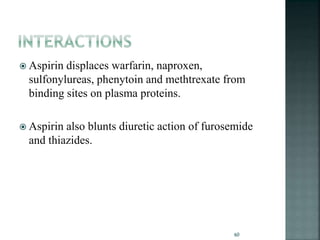
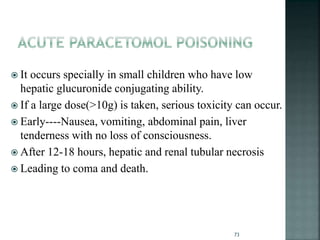
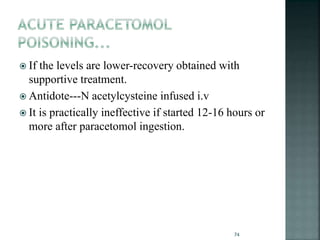
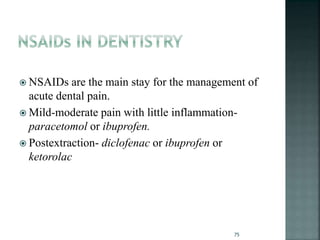
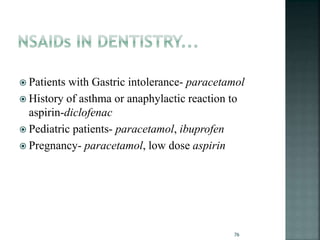
This document provides an overview of analgesics (painkillers) including their classification, mechanisms of action, adverse effects, uses, and addiction potential. It focuses on opioid analgesics such as morphine, codeine, heroin, pethidine, and tramadol which are derived from the opium poppy. It discusses the history of opioid use and trade dating back thousands of years. It also covers non-opioid options like NSAIDs, acetaminophen, and various opioid antagonists used to treat overdose and addiction. The document aims to educate on the appropriate use and risks of different analgesic drugs.