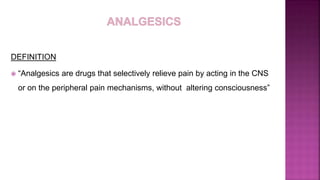
Dr Nazam Tafadar presented on analgesics and NSAIDs. Key points included:
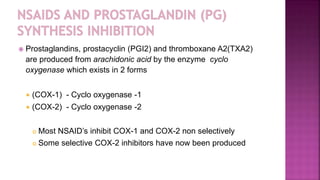
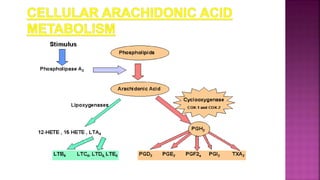
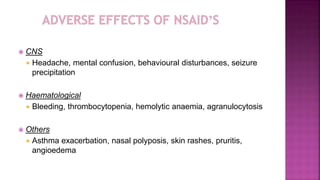
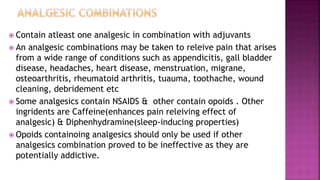
- Analgesics are drugs that selectively relieve pain without altering consciousness. NSAIDs relieve pain and reduce inflammation by inhibiting cyclooxygenase enzymes.
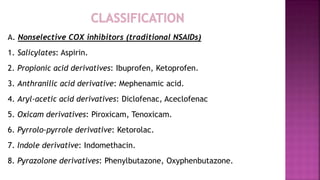
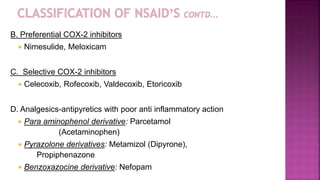
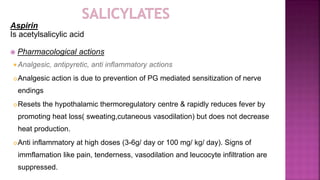
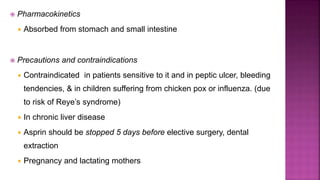
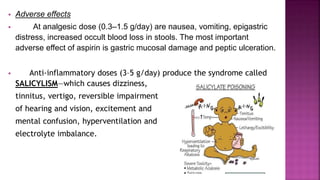
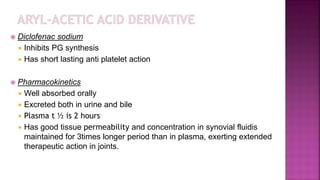
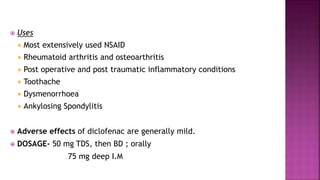
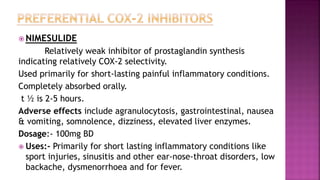
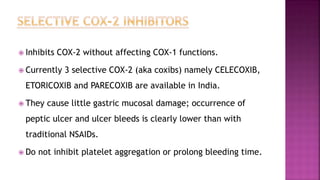
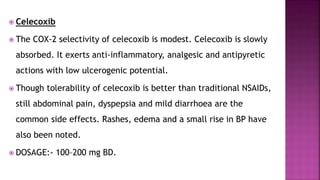
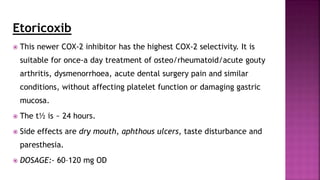
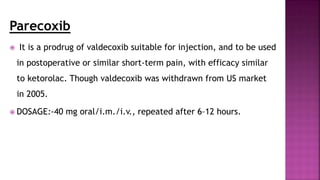
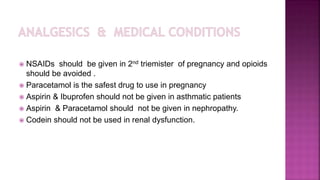
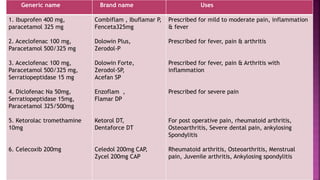
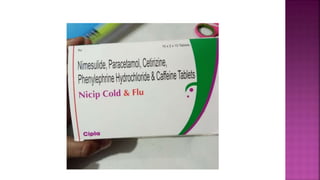
- Common NSAIDs include aspirin, ibuprofen, diclofenac, and nimesulide. Selective COX-2 inhibitors like celecoxib have fewer gastrointestinal side effects.
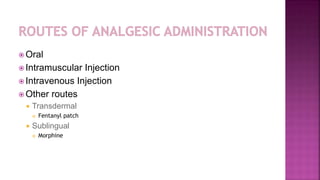
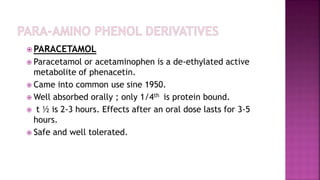
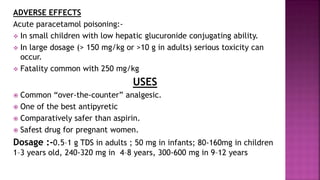
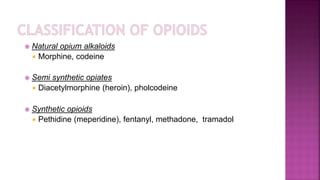
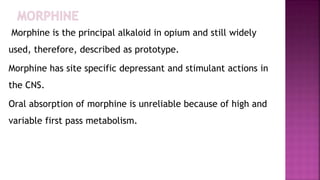
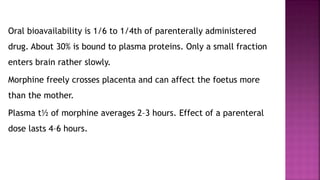
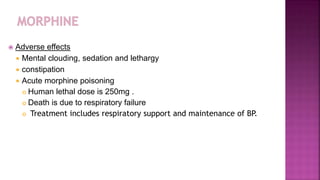
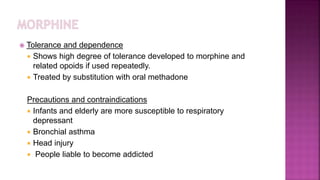
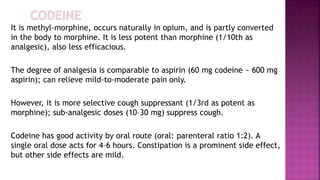
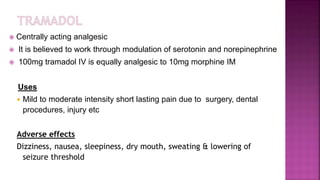
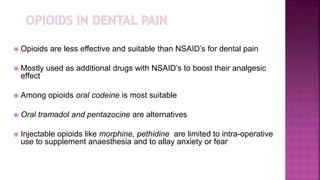
- Paracetamol is a commonly used over-the-counter analgesic with few side effects. Opioids are another class of analgesics that includes morphine, codeine, and fentanyl patches.