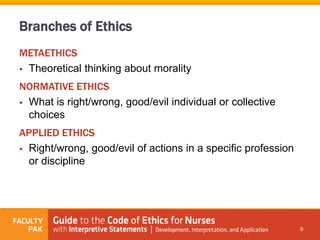
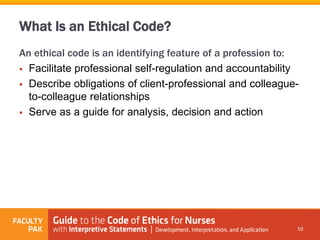
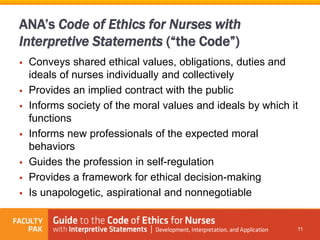
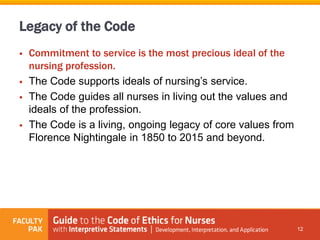
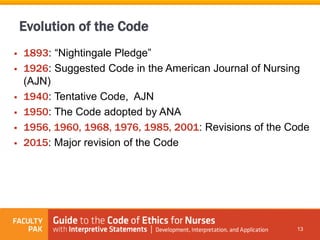
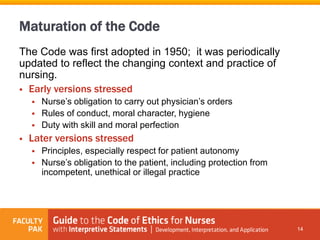
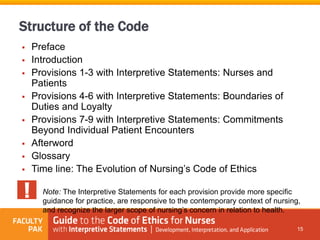
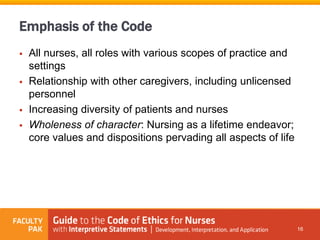
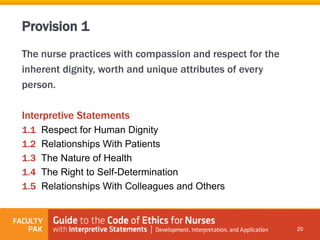
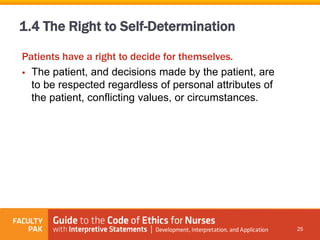
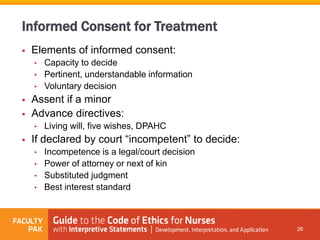
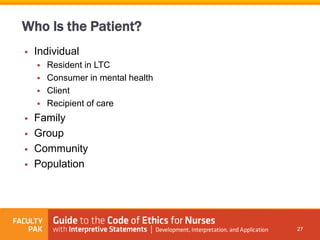
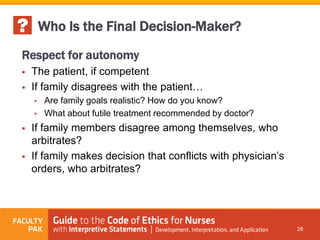
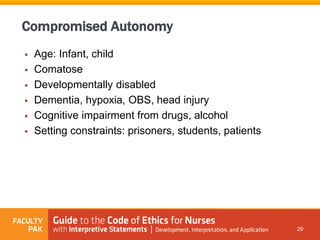
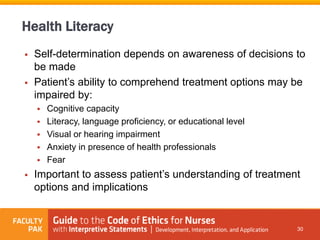
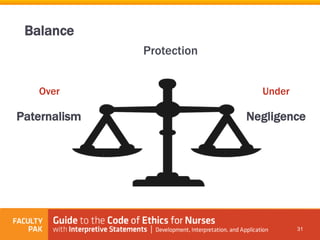
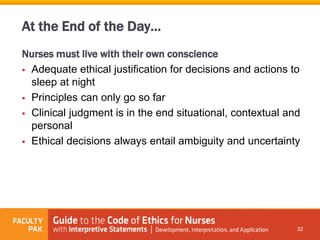
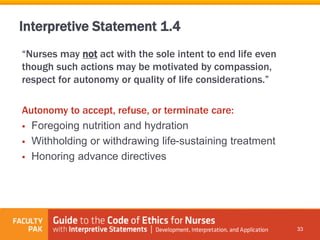
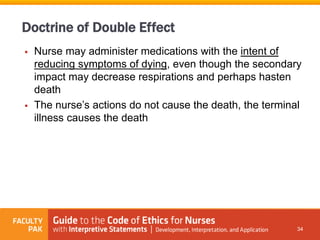
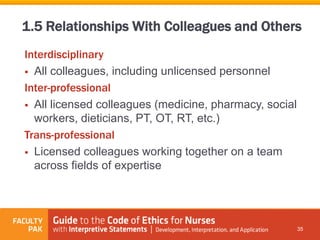
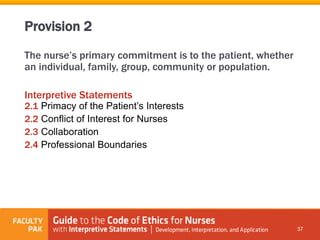
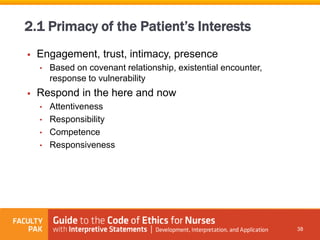
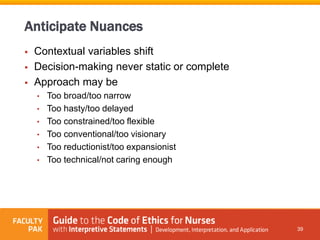
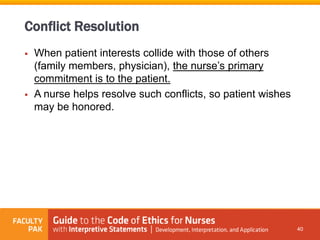
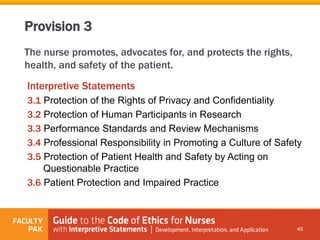
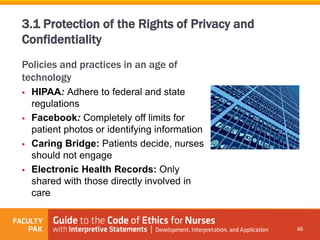
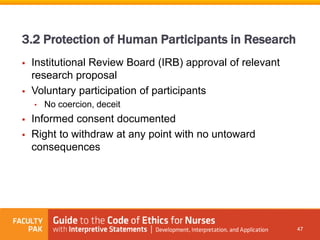
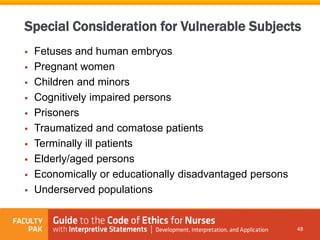
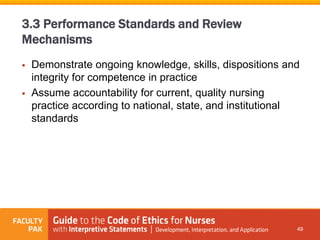
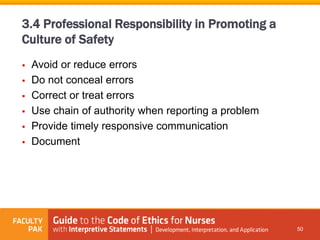
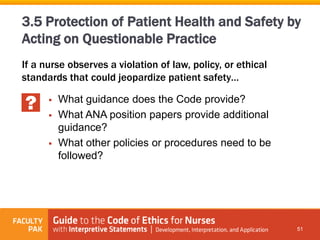
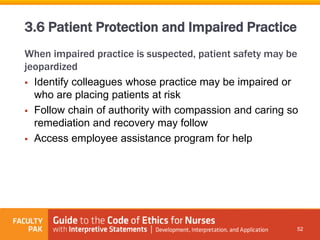
The document provides an overview of the Code of Ethics for Nurses and its provisions related to nurses and patients. It discusses how the Code evolved over time and now emphasizes respect for patient dignity and autonomy. It also describes the nurse's primary commitment to the patient in terms of privacy, informed consent, conflicts of interest, and promoting safety. The document is intended to educate nurses about their ethical obligations according to the Code.