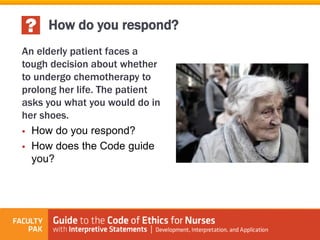
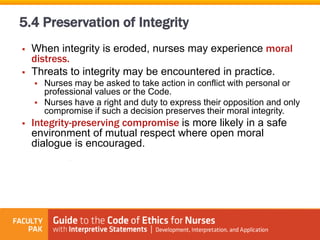
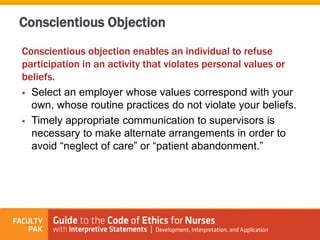
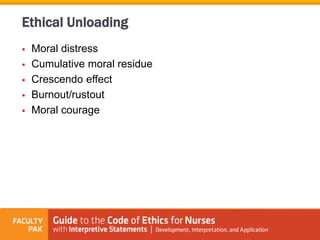
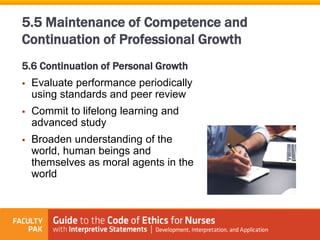
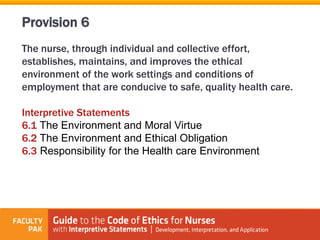
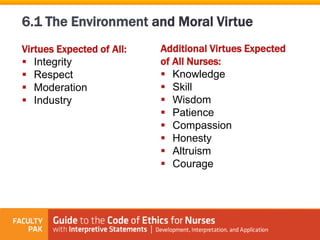
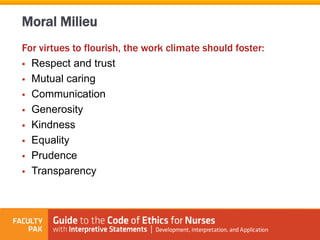
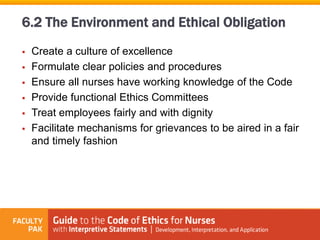
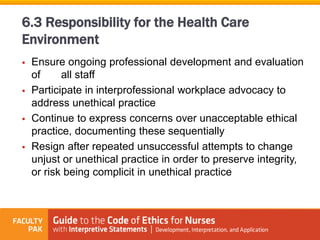
This document discusses provisions 4-6 from the American Nurses Association Code of Ethics, which focus on nurses' responsibilities and accountability in practice. Provision 4 discusses a nurse's authority over their own practice and maintaining competence. Provision 5 discusses duties to oneself, including self-care, integrity, and continuing education. Provision 6 discusses establishing an ethical work environment through collaborative efforts to shape a culture that fosters ethical integrity.