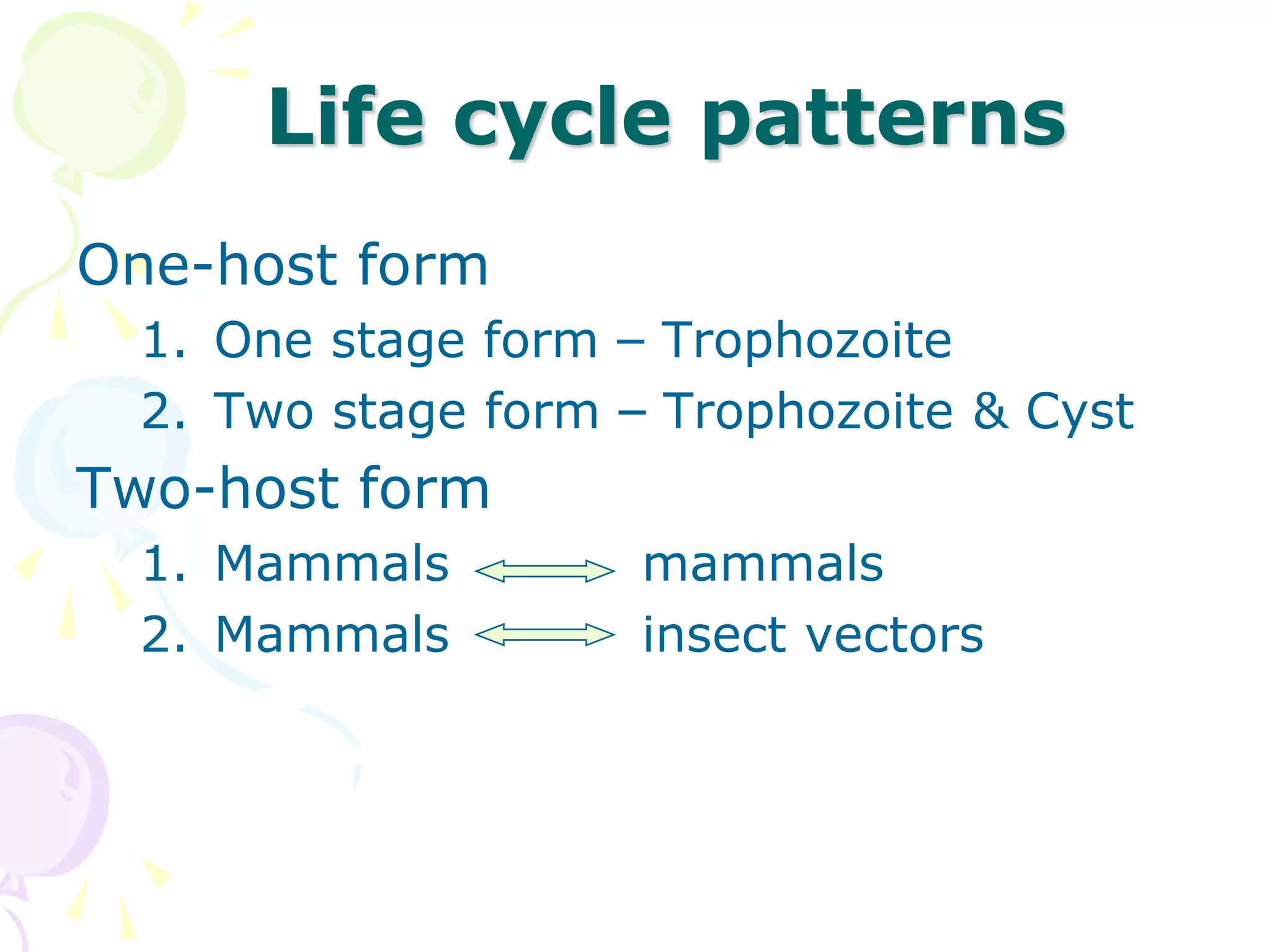
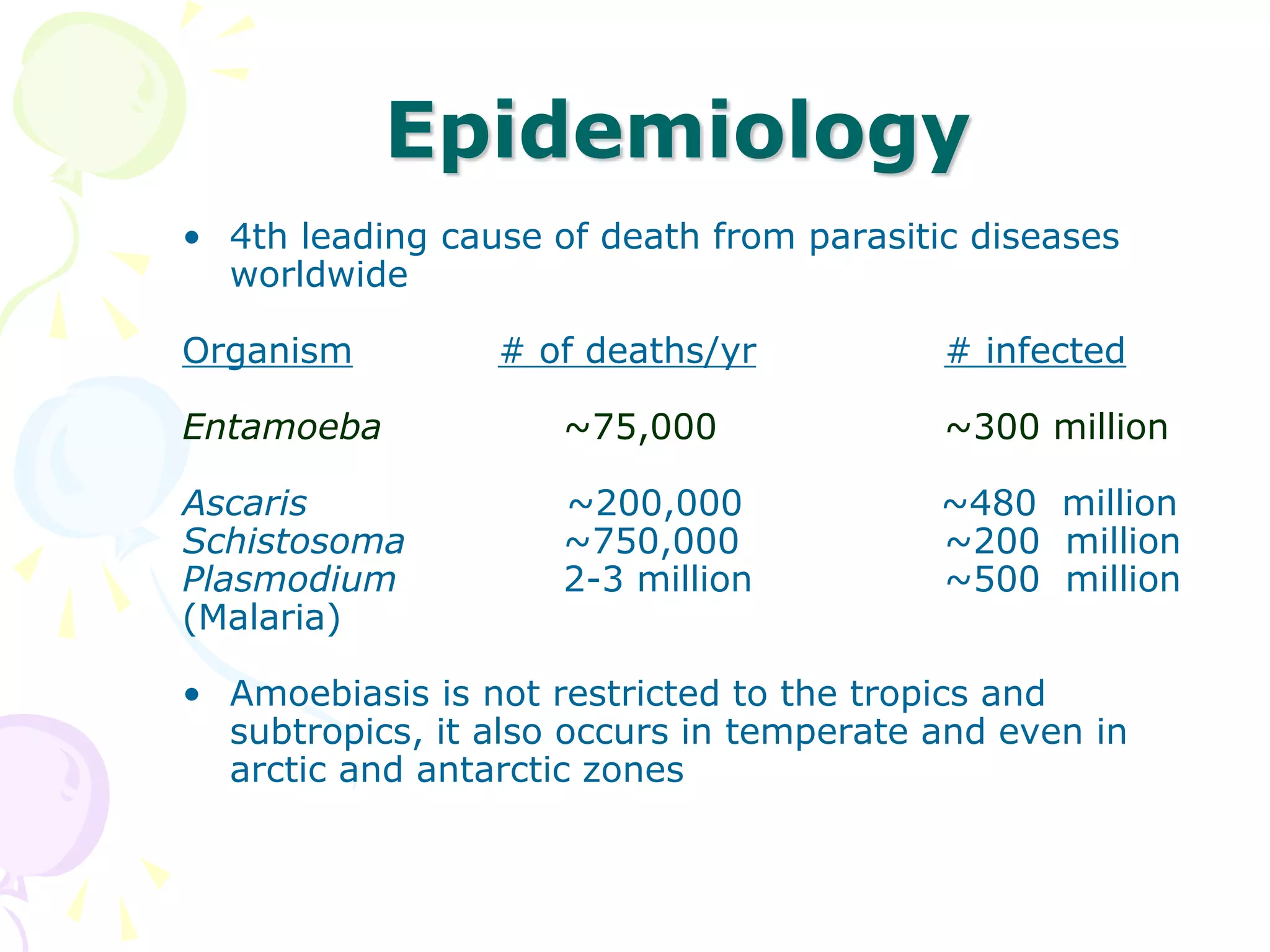
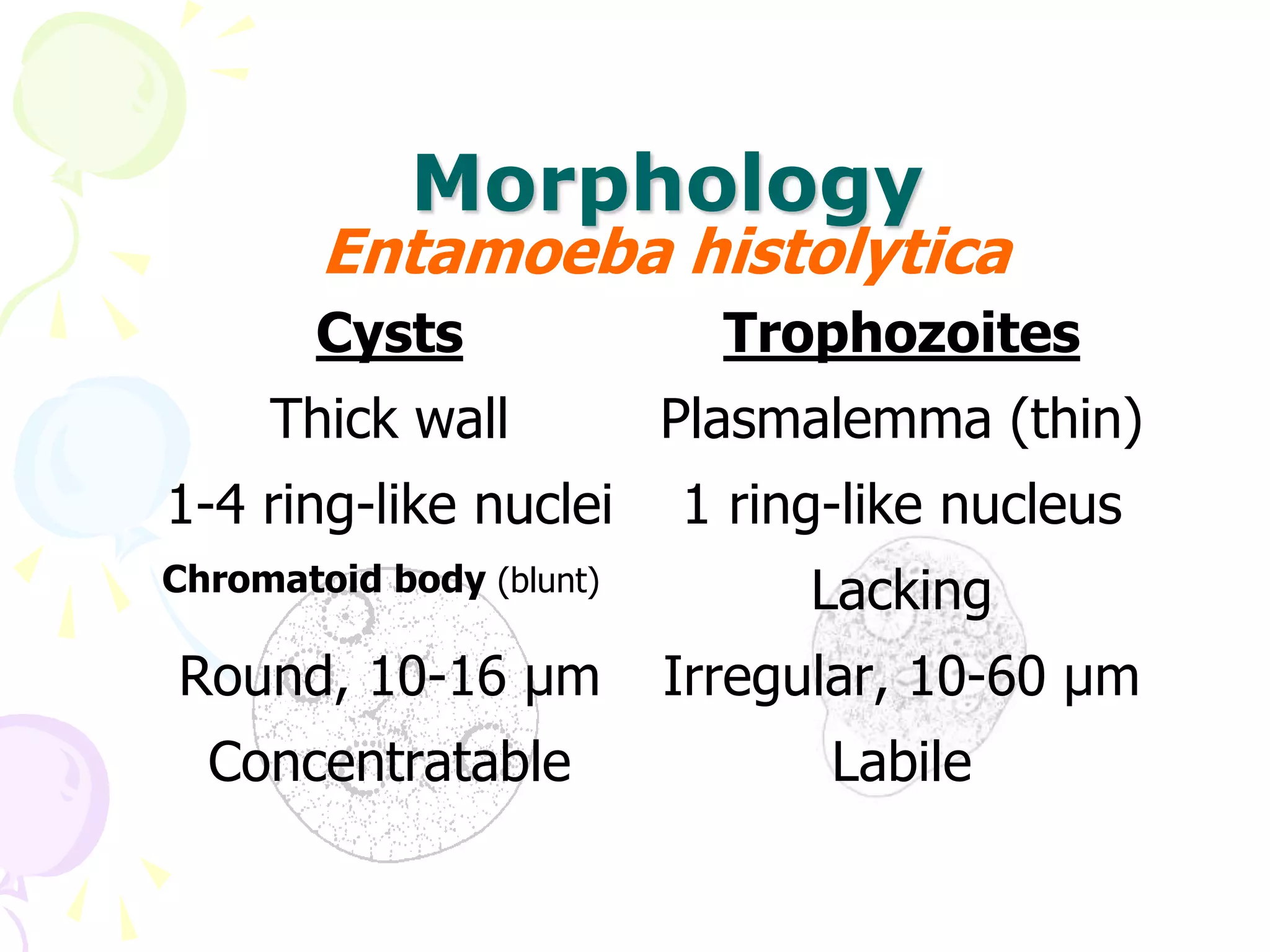
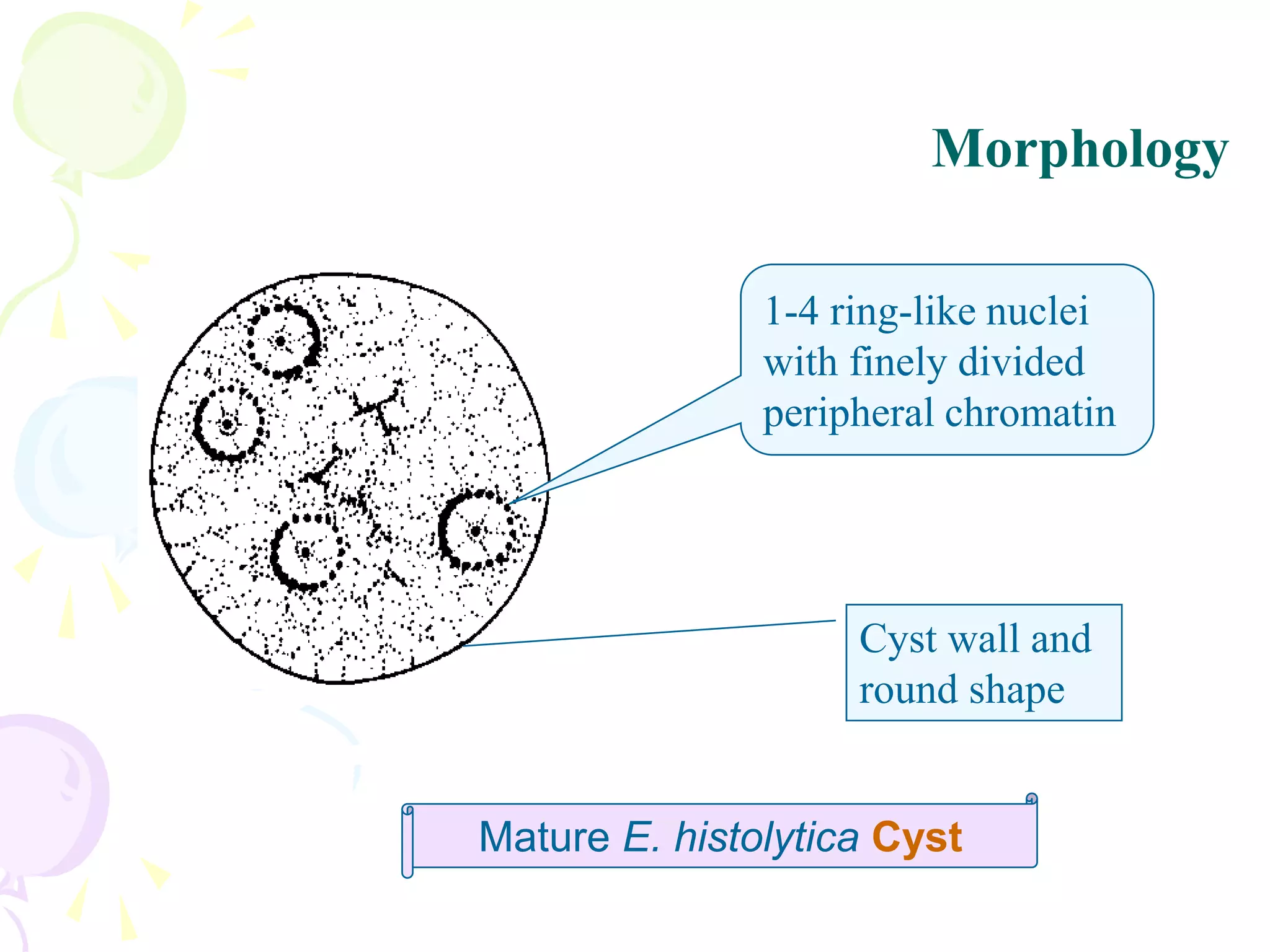
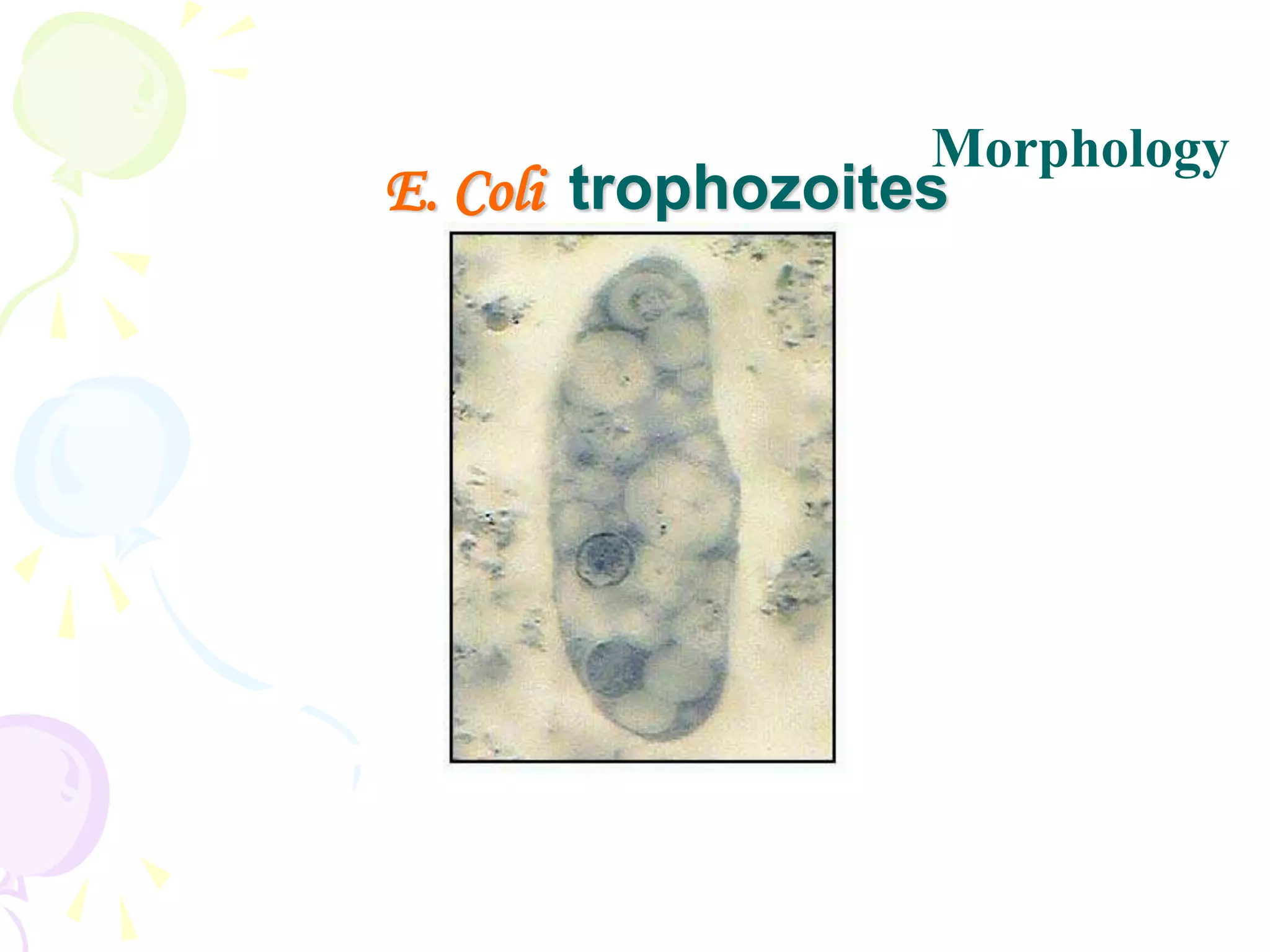
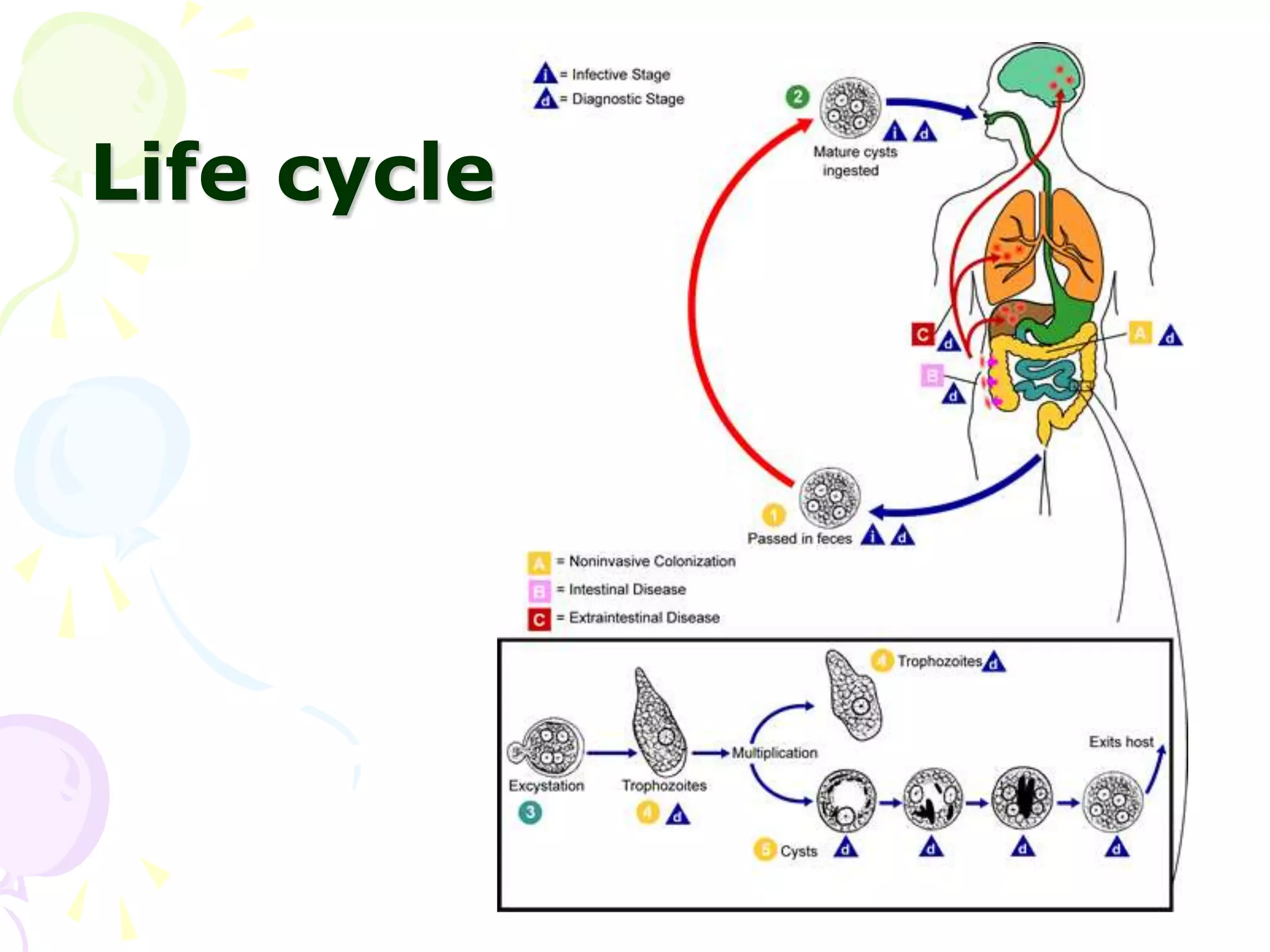
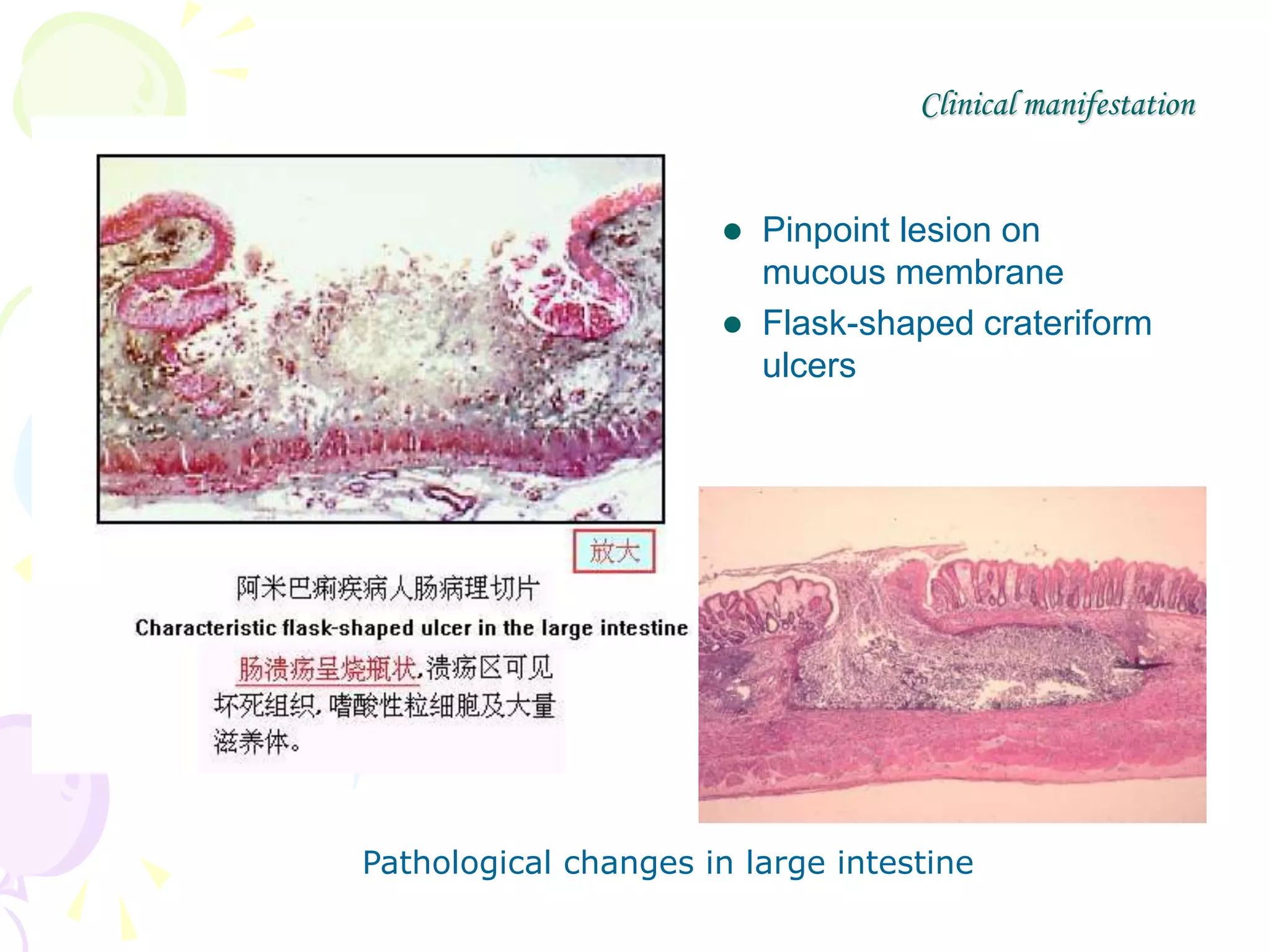
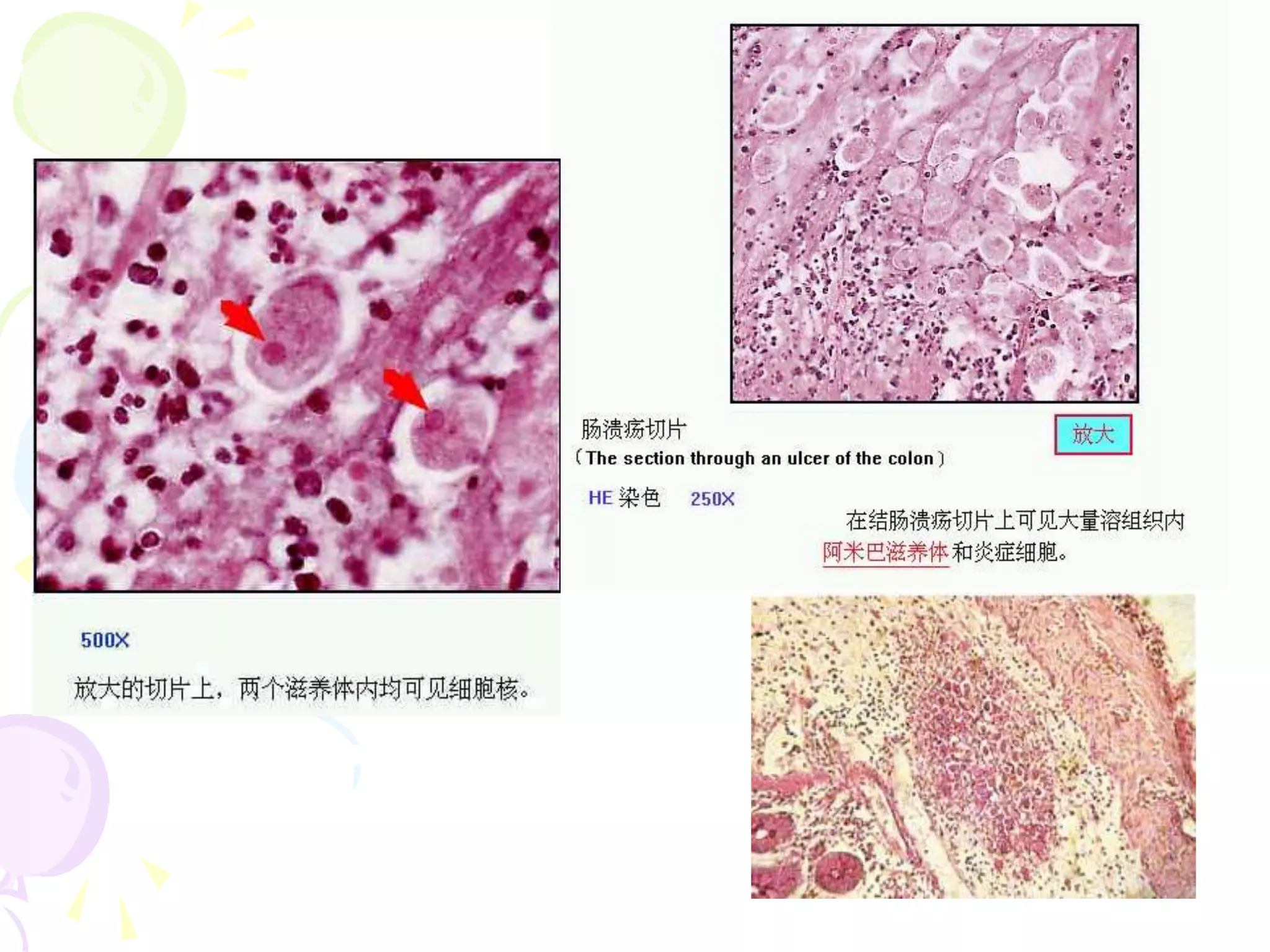
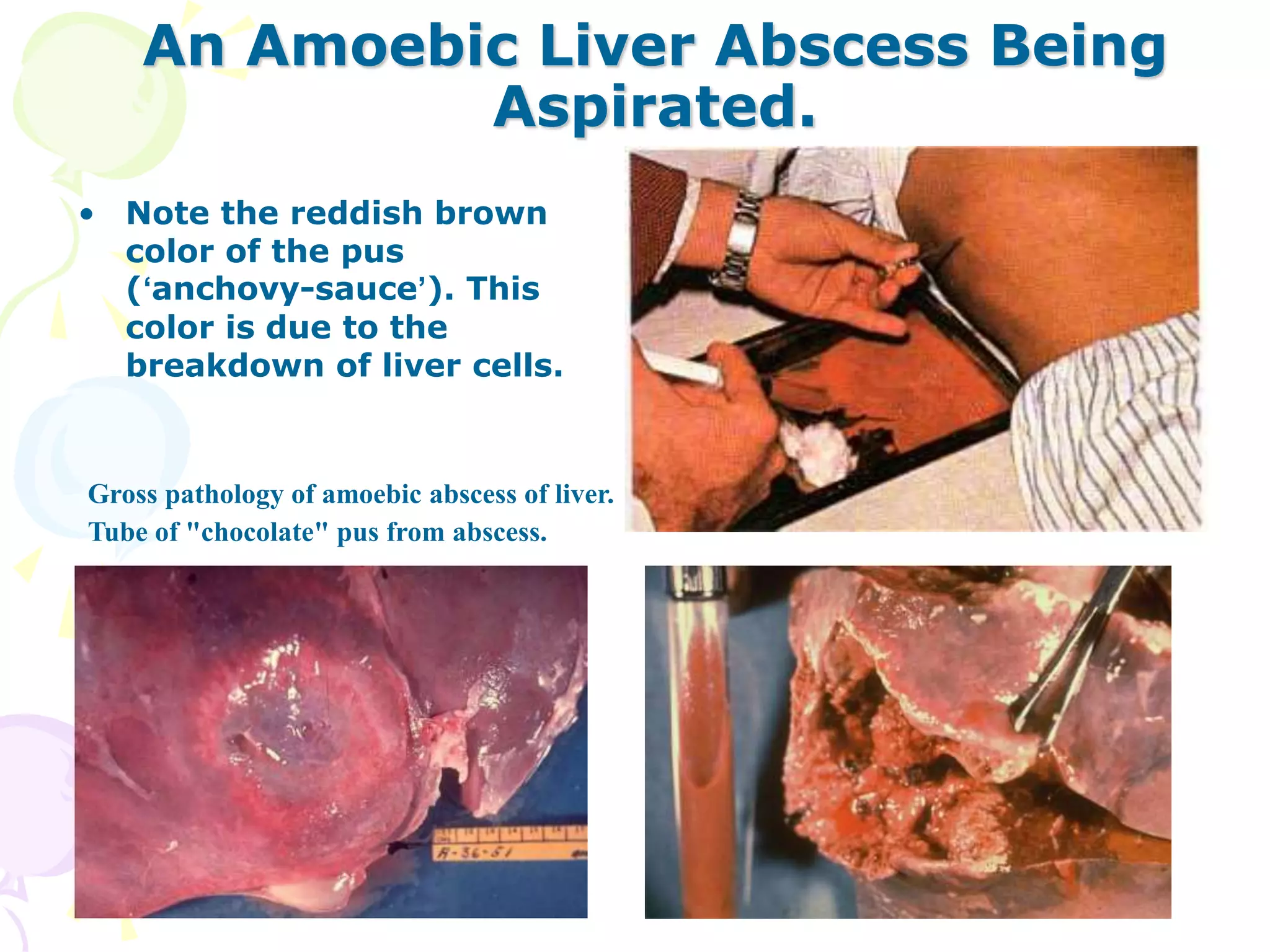
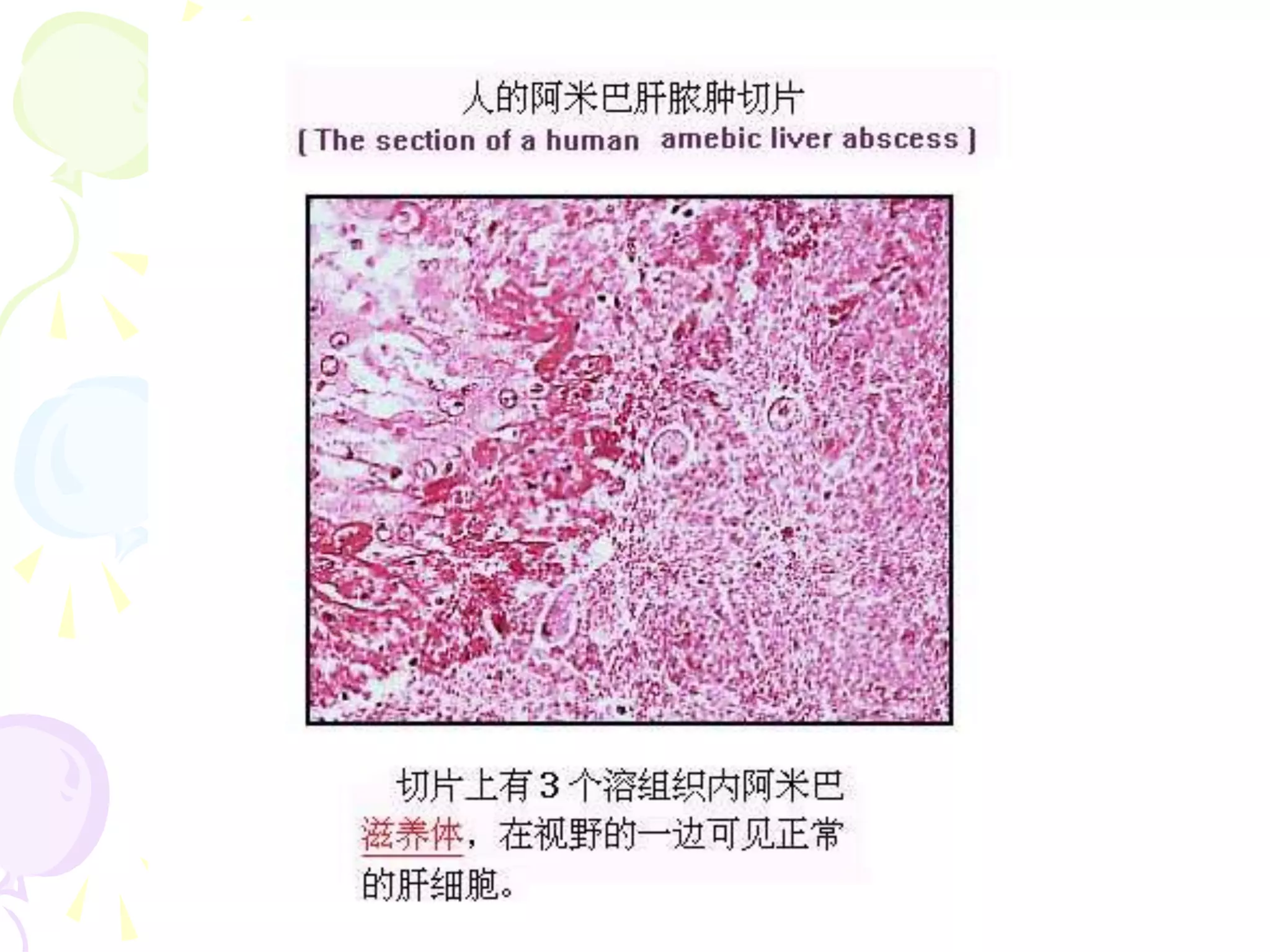
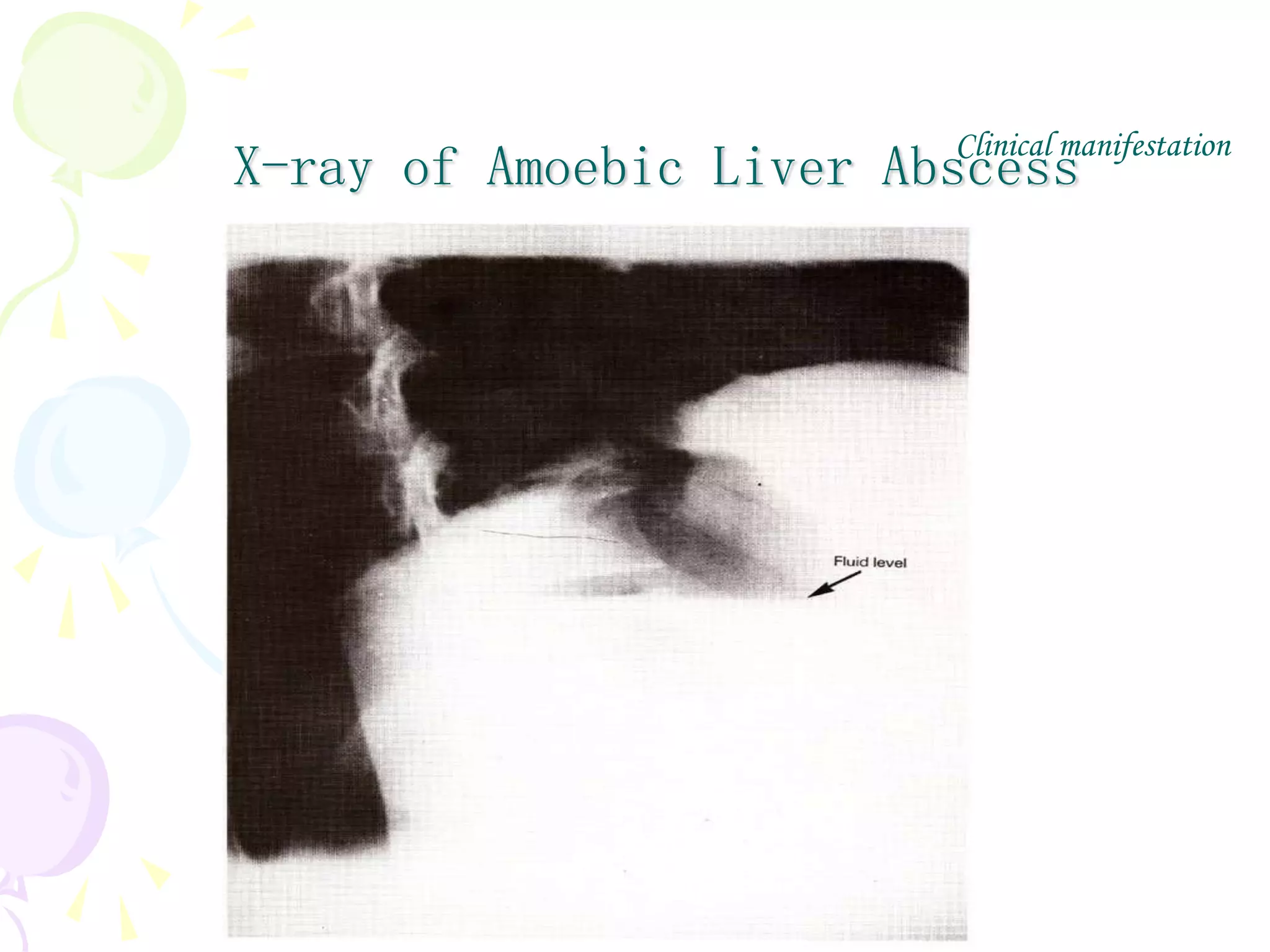
Protozoa are single-celled eukaryotic organisms classified into groups including amoebas, flagellates, and ciliates. The document discusses Entamoeba histolytica, the causative agent of amoebiasis. E. histolytica has a life cycle involving an infective cyst stage and invasive trophozoite stage. It is transmitted via the fecal-oral route in areas with poor sanitation. Amoebiasis ranges from asymptomatic carriage to acute dysentery and extra-intestinal infections like amoebic liver abscess. Diagnosis involves stool examination for cysts and trophozoites. Treatment depends on the infection stage and severity.