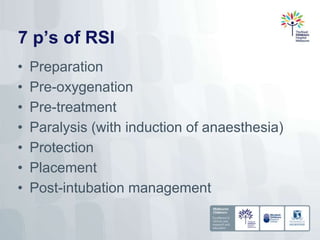
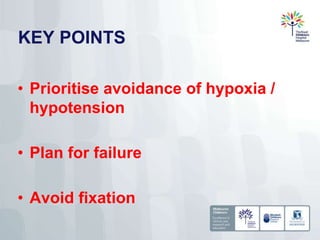
This document discusses improving safety during emergency airway management. It outlines strategies like prioritizing avoidance of hypoxia and hypotension, planning for failure, avoiding fixation on intubation, pre-oxygenation, apneic oxygenation, and using capnography to confirm proper placement and avoid complications. Emergency department and ICU intubations carry the highest risk. The author advocates for governance, standardized equipment and checklists, training, and regular audits to continuously improve outcomes and work towards zero preventable harm during emergency airway procedures.