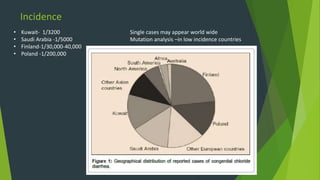
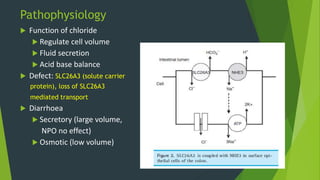
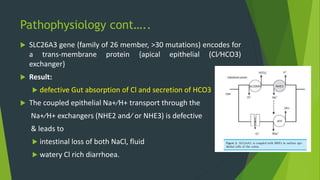
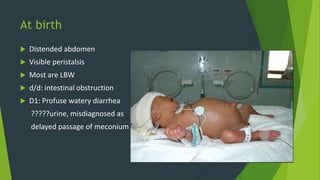
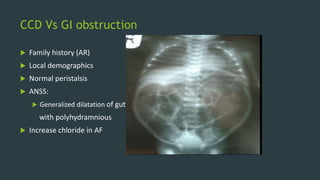
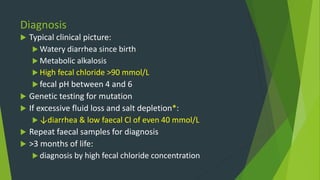
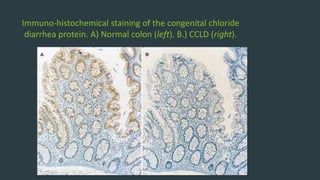
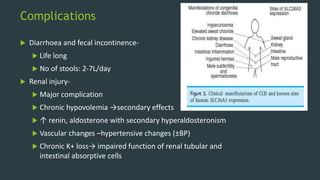
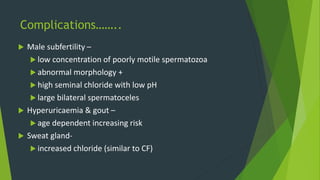
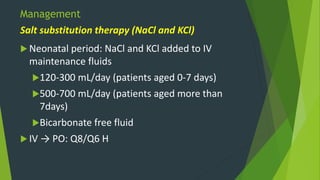
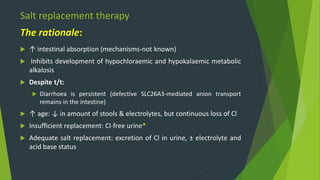
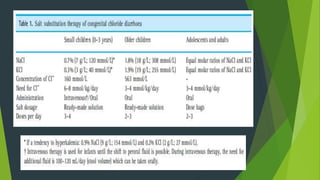
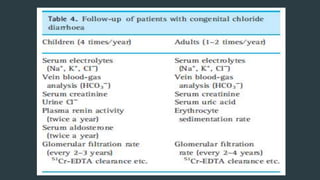
This document discusses chloride losing diarrhoea (CLD), a rare genetic condition caused by mutations in the SLC26A3 gene. It causes watery diarrhoea from birth and metabolic alkalosis due to excessive chloride loss. It can lead to dehydration, electrolyte imbalances, and long-term complications affecting the kidneys and male fertility if not properly managed. Treatment involves oral and intravenous salt replacement therapy with sodium chloride and potassium chloride to prevent complications from hypochloraemia and hypokalemia. Additional treatments including proton pump inhibitors, oral butyrate, and cholestyramine may help reduce diarrhoea. With prompt treatment and management of electrolyte losses, outcomes have improved from