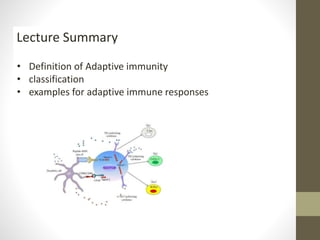
Adaptive immunity develops in response to stimuli that induce antibody production. It has two main branches: active immunity and passive immunity. Active immunity involves the immune system developing its own response through infection or vaccination, resulting in immunological memory. Passive immunity involves receiving ready-made antibodies from another source, providing immediate but temporary protection without memory. Adaptive immunity is classified as actively or passively acquired, with actively acquired immunity developing through natural exposure or vaccination, while passively acquired immunity results from maternal antibody transfer or immunoglobulin administration.