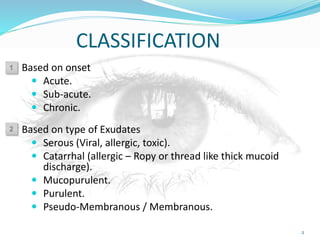
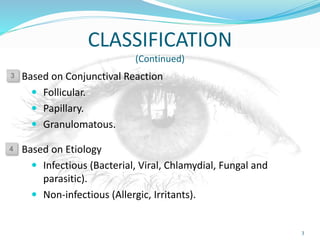
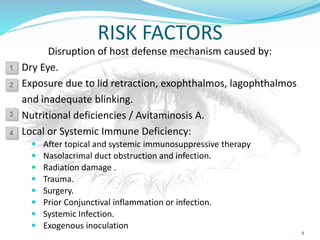
This document discusses the classification and types of acute conjunctivitis. It is classified based on onset (acute, sub-acute, chronic), type of exudate (serous, catarrhal, mucopurulent, purulent, pseudo-membranous), and etiology (infectious, non-infectious). The types discussed include bacterial (purulent, gonococcal, membranous, angular), viral, chlamydial, and ophthalmia neonatorum. For each type, the etiology, clinical features, complications, and treatment are described. Risk factors like dry eye, nutritional deficiencies, and immune deficiencies that can lead to acute conjunctivitis are also outlined