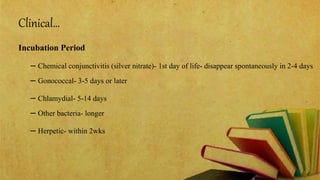
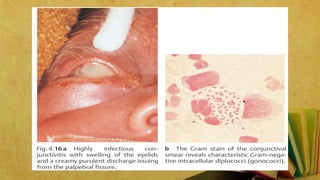
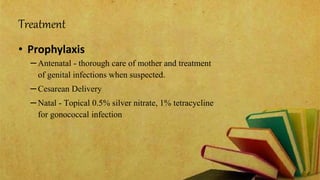
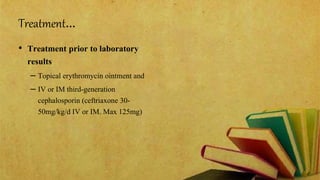
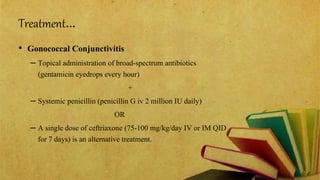
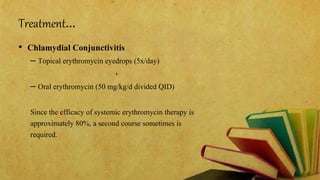
This document discusses ophthalmia neonatorum, which is inflammation of the conjunctiva in newborns during the first 28 days of life. It can be caused by infection transmitted from the mother's birth canal. Without silver nitrate eye drops, 10-15% of newborns were infected historically. Today the most common causes are Chlamydia trachomatis and Neisseria gonorrhoeae. Symptoms vary but include eye redness, swelling, and discharge. Treatment involves topical and sometimes systemic antibiotics. Proper prenatal care and treatment of maternal infections can help prevent this condition.