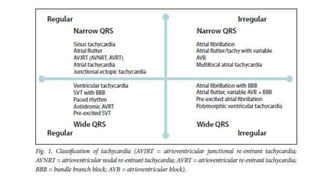
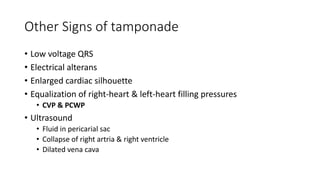
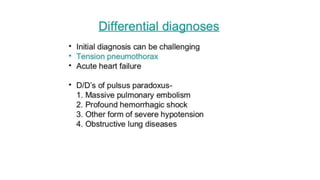
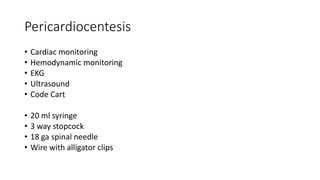
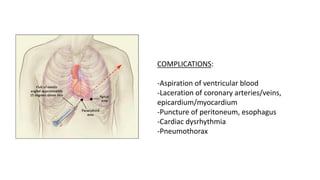
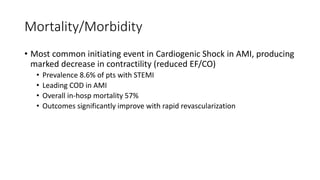
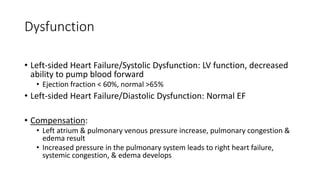
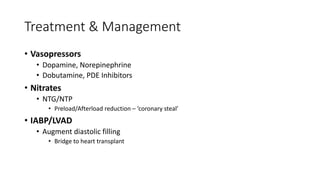
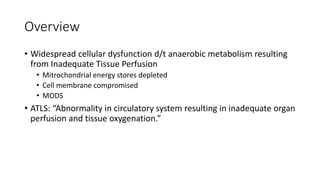
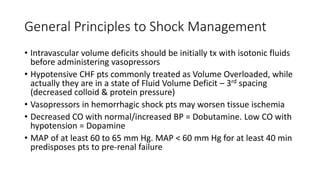
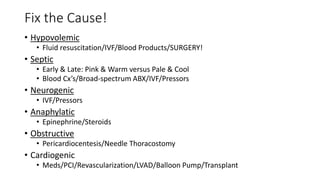
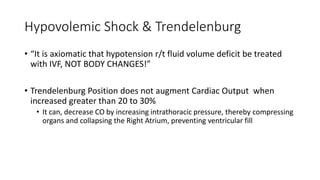
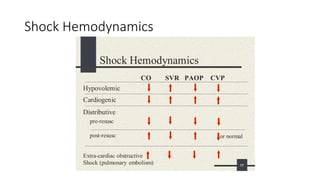
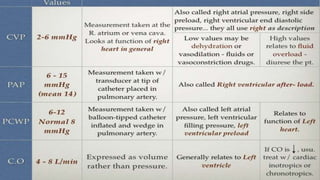
The document provides an overview of the management of acute cardiovascular disorders including sudden cardiac arrest, shock, heart failure, pericardial tamponade, and dysrhythmias. Key points discussed include the importance of high-quality CPR with minimal interruptions, use of epinephrine and vasopressors in cardiac arrest and shock, identification and treatment of different shock types, and techniques for pericardiocentesis. General principles of shock management are outlined focusing on initial volume resuscitation and considering the cause of shock when determining appropriate treatment.