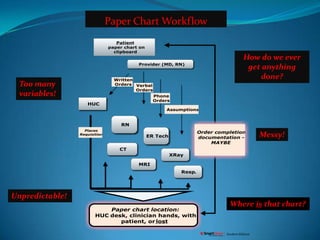
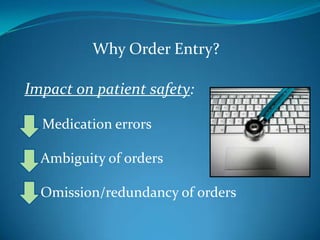
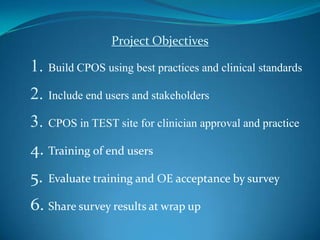
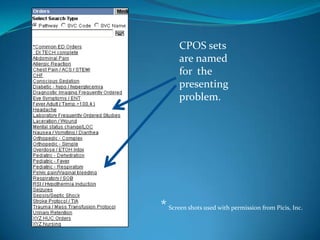
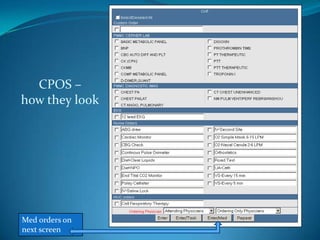
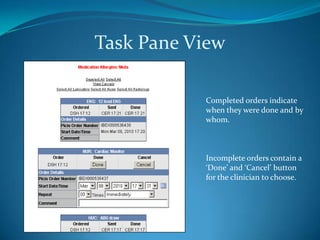
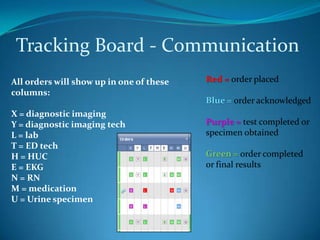
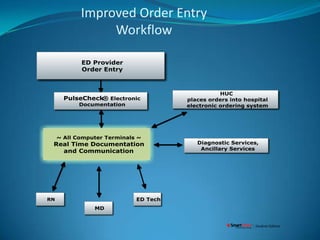
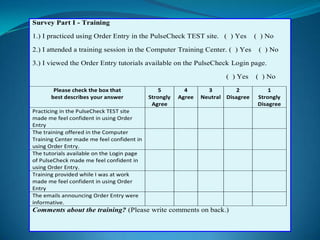
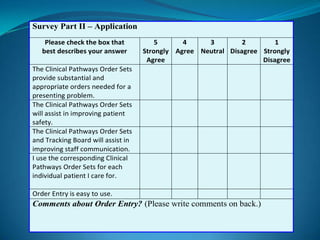
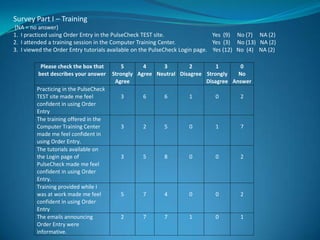
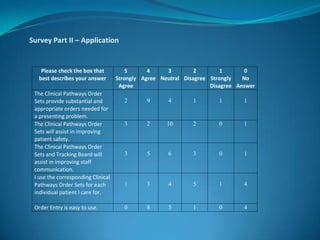
The document outlines the development and implementation of customized Clinical Pathway Order Sets (CPOS) to replace handwritten orders in the emergency department, addressing issues of medical errors and communication inefficiencies. Project objectives included building CPOS based on best practices, training end users, and evaluating acceptance through surveys, which revealed mixed feelings about the usefulness of the order sets among nursing staff. Although training ratings were generally positive, concerns about the order sets being primarily for physicians could hinder their successful adoption.

![ReferencesFarrell, A. (2008, Nov. 13). Preparing for clinical documentation: A strategic view [webinar]. Healthcare Information and Management Systems Society (HIMSS). Retrieved from http://www.himss.orgLee, P. D., and Hirshfield, M. (2006). Project planning for healthcare. The Health Care Manager, 25 (4), 310-314.Mewshaw, M. R., White, K. M., and Walrath, J. (2006, October). Medical errors: Where are we now? Nursing Management, 37(10), pp. 50–54.Piechowski, R. (2006). Making CPOE work: Redesign workflows to optimize benefits. Patient Safety & Quality Healthcare, March/April. Retrieved from http://www.psqh.com/marapr06/cpoe.htmlSengstack, P. P. and Gugerty, B. (2004, Winter). CPOE systems: Success factors and implementation issues. Journal of Healthcare Information Management, 18 (1), pp. 36-45.](https://image.slidesharecdn.com/publicpresentcpos-12788684592739-phpapp01/85/Building-Customized-Clinical-Pathway-Order-Sets-for-CPOE-Implementation-20-320.jpg)