This document provides an overview of asthma pathophysiology, medications, and management for a pediatric/PICU fellowship. Key points include:
- Controlling asthma requires differentiating between rescue and controller medications and identifying triggers.
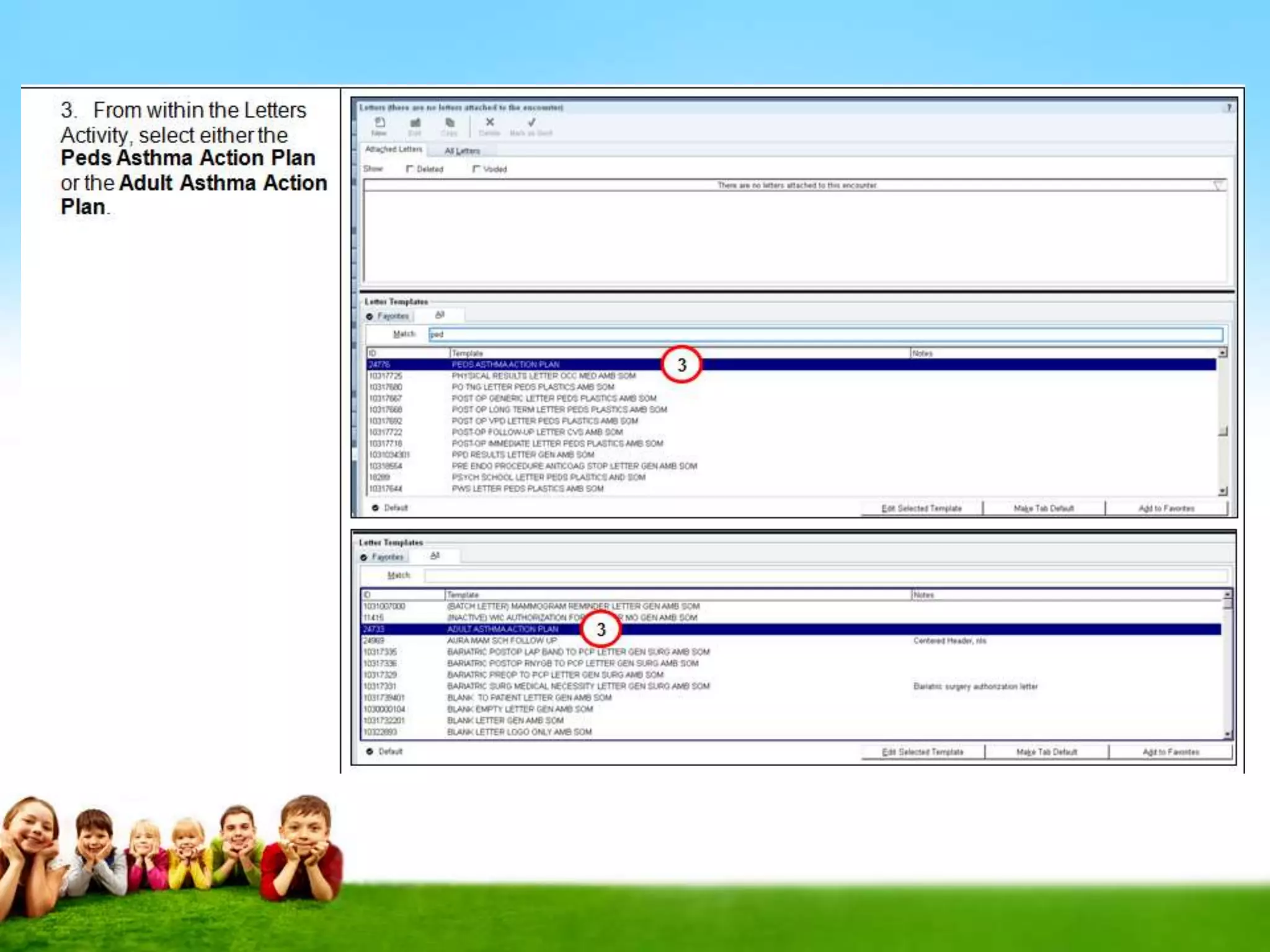
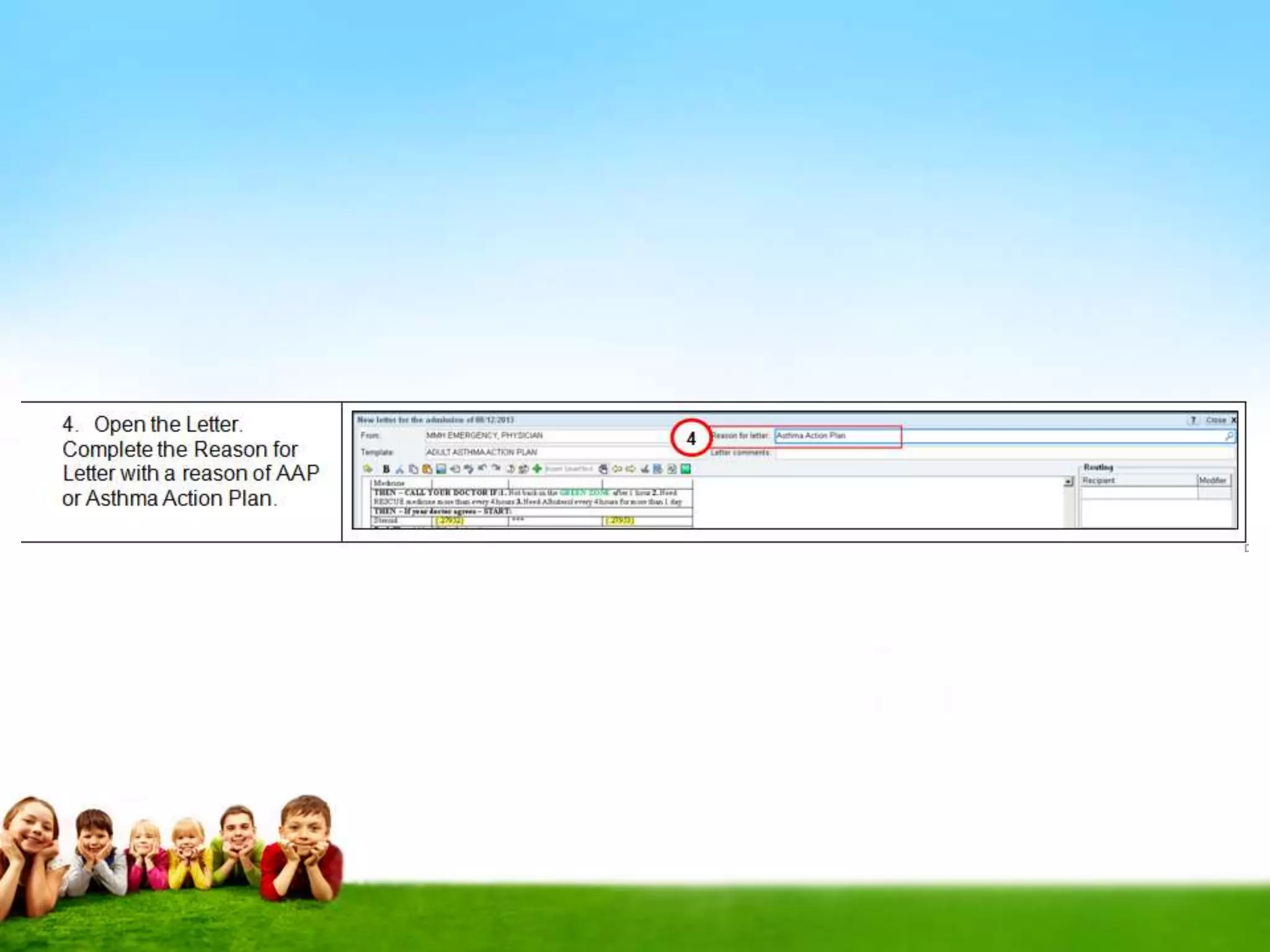
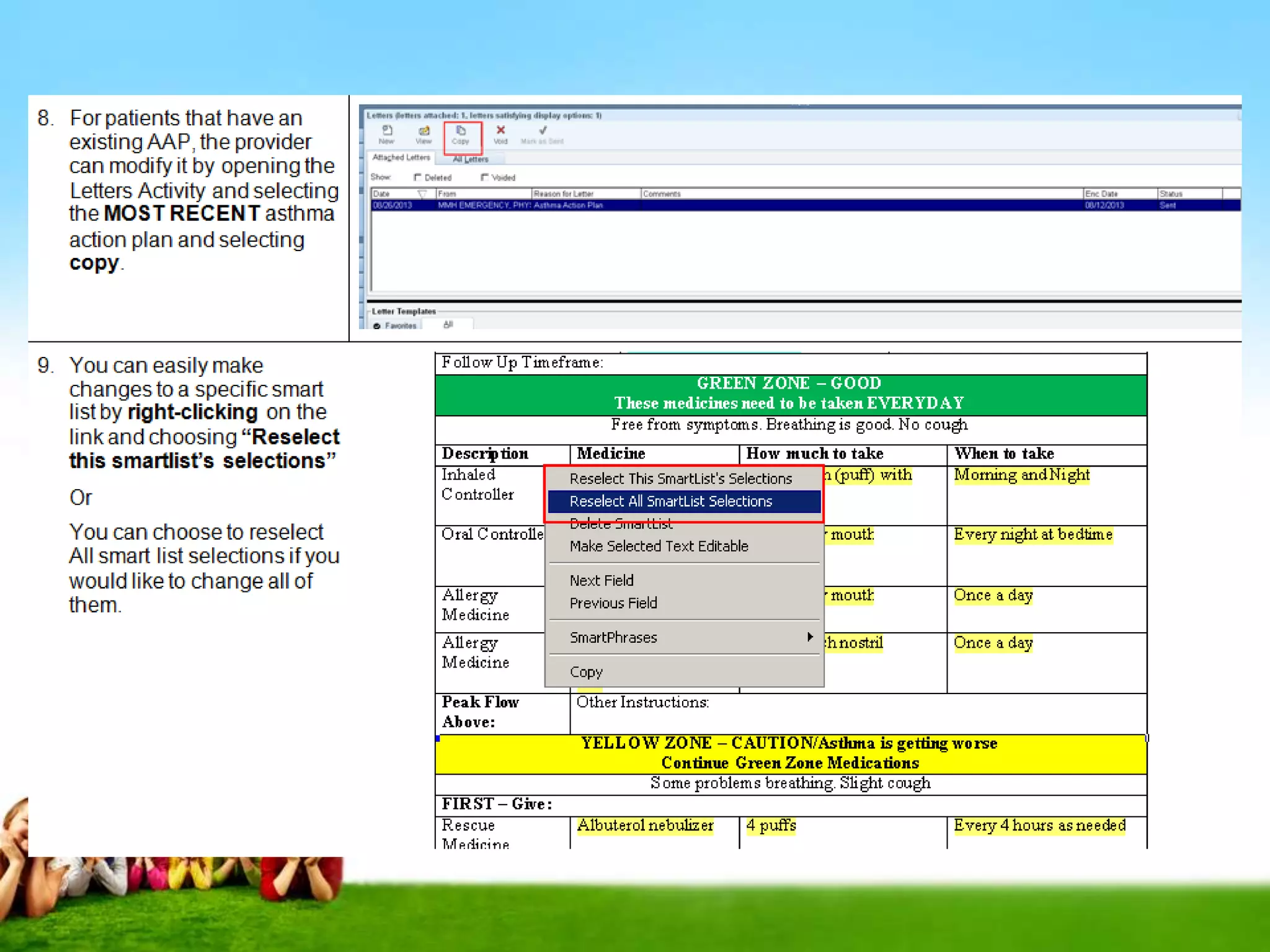
- Asthma action plans are crucial for self-management but often lacking in detail or not utilized.
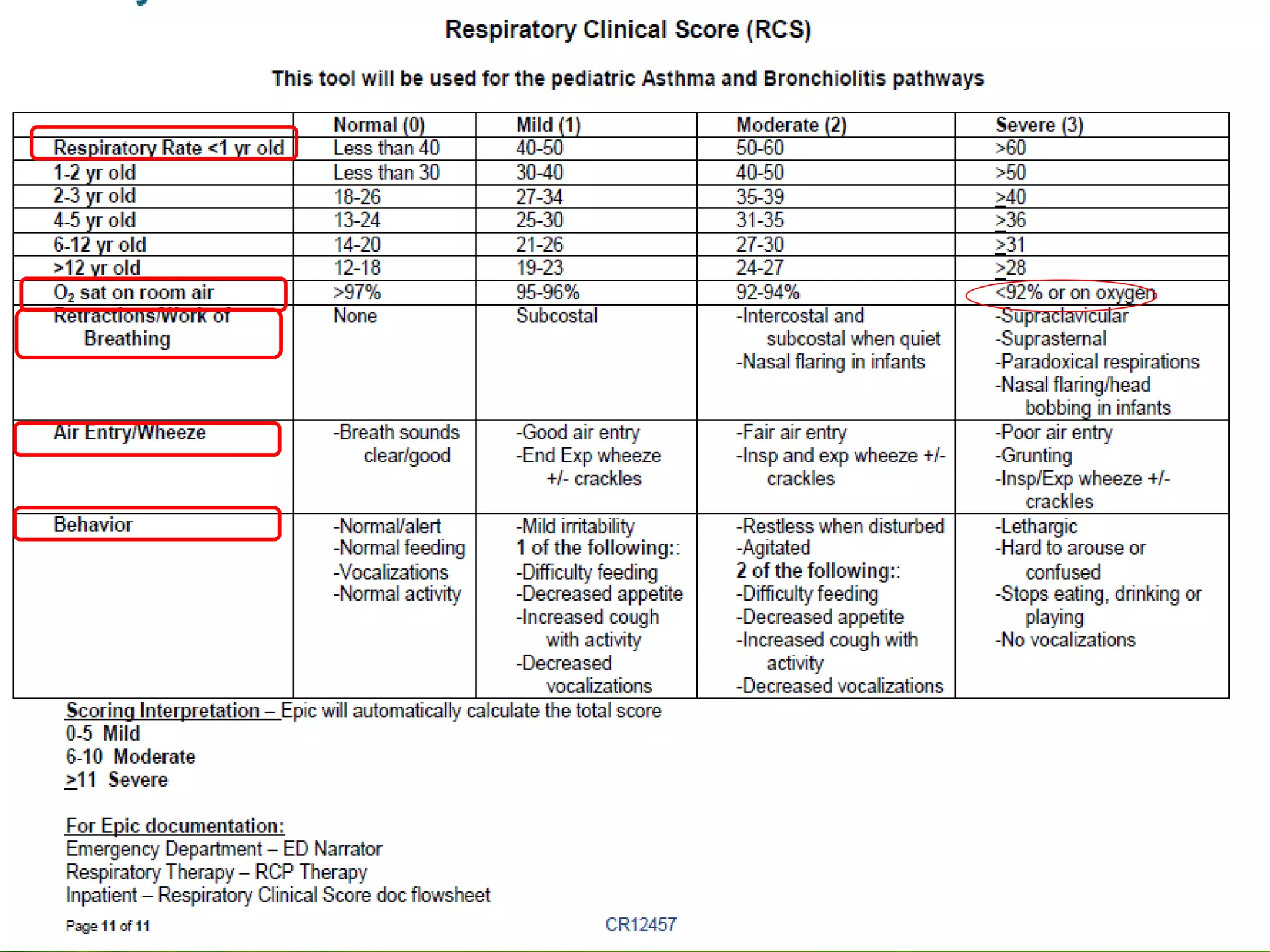
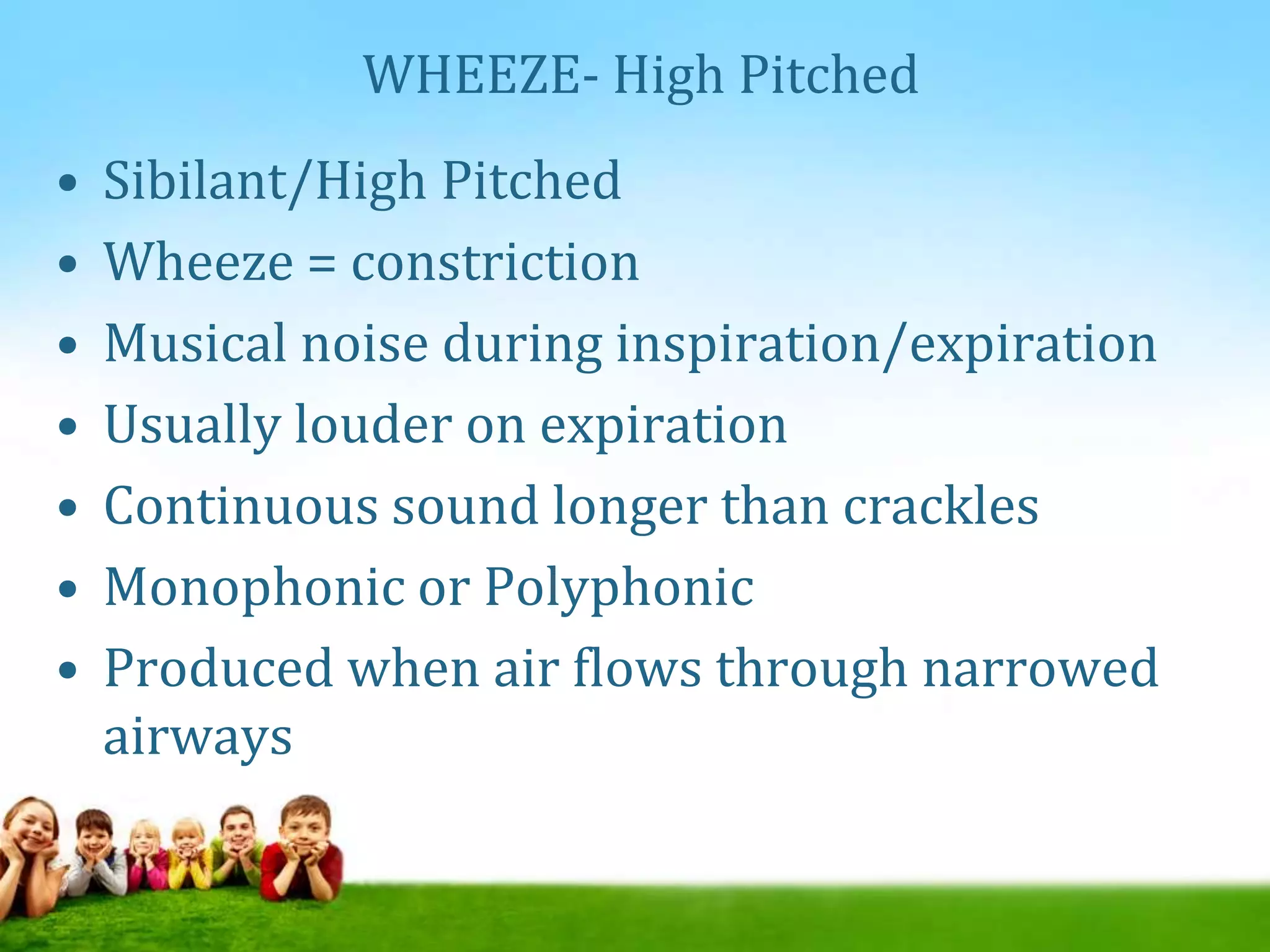
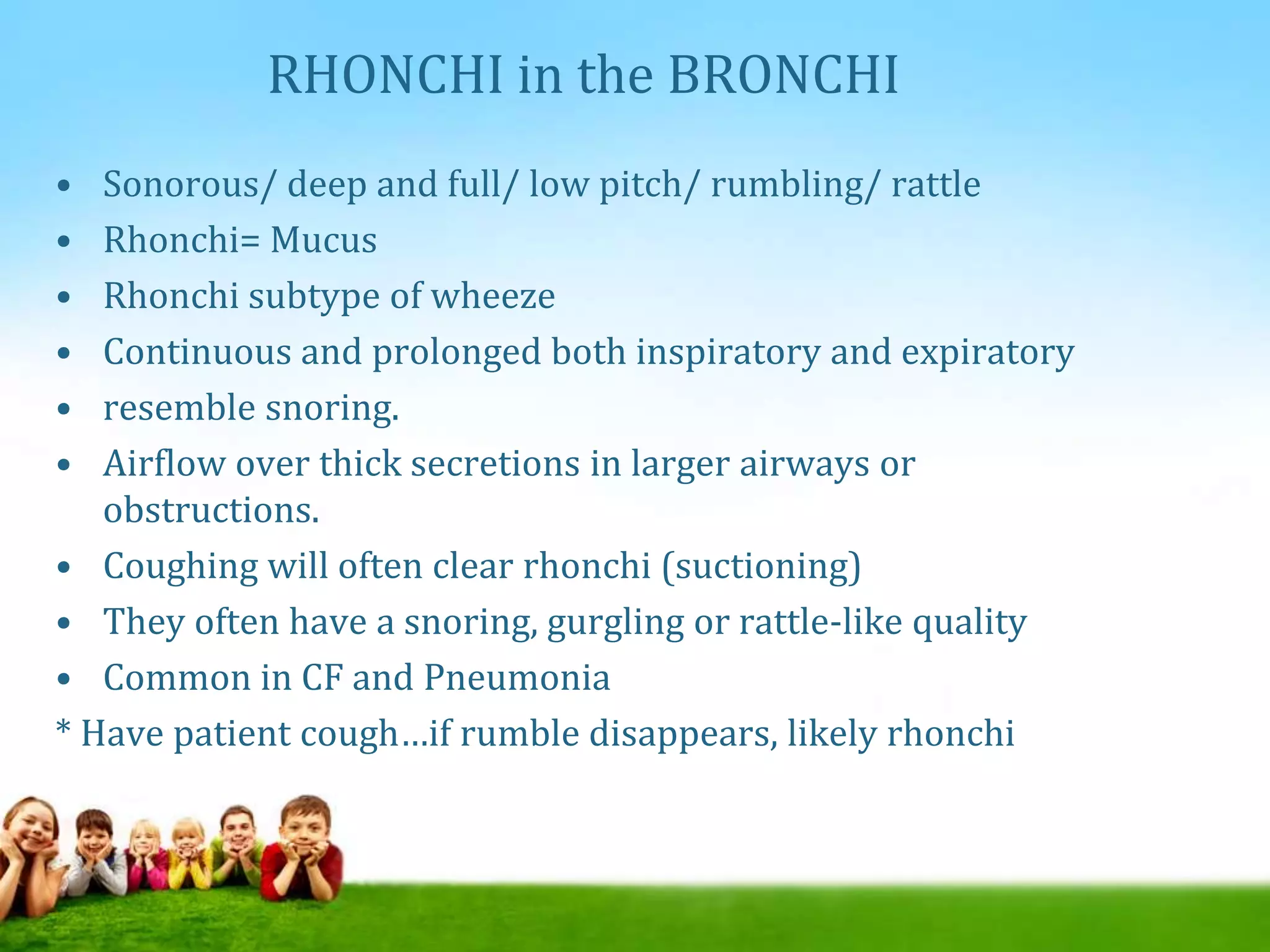
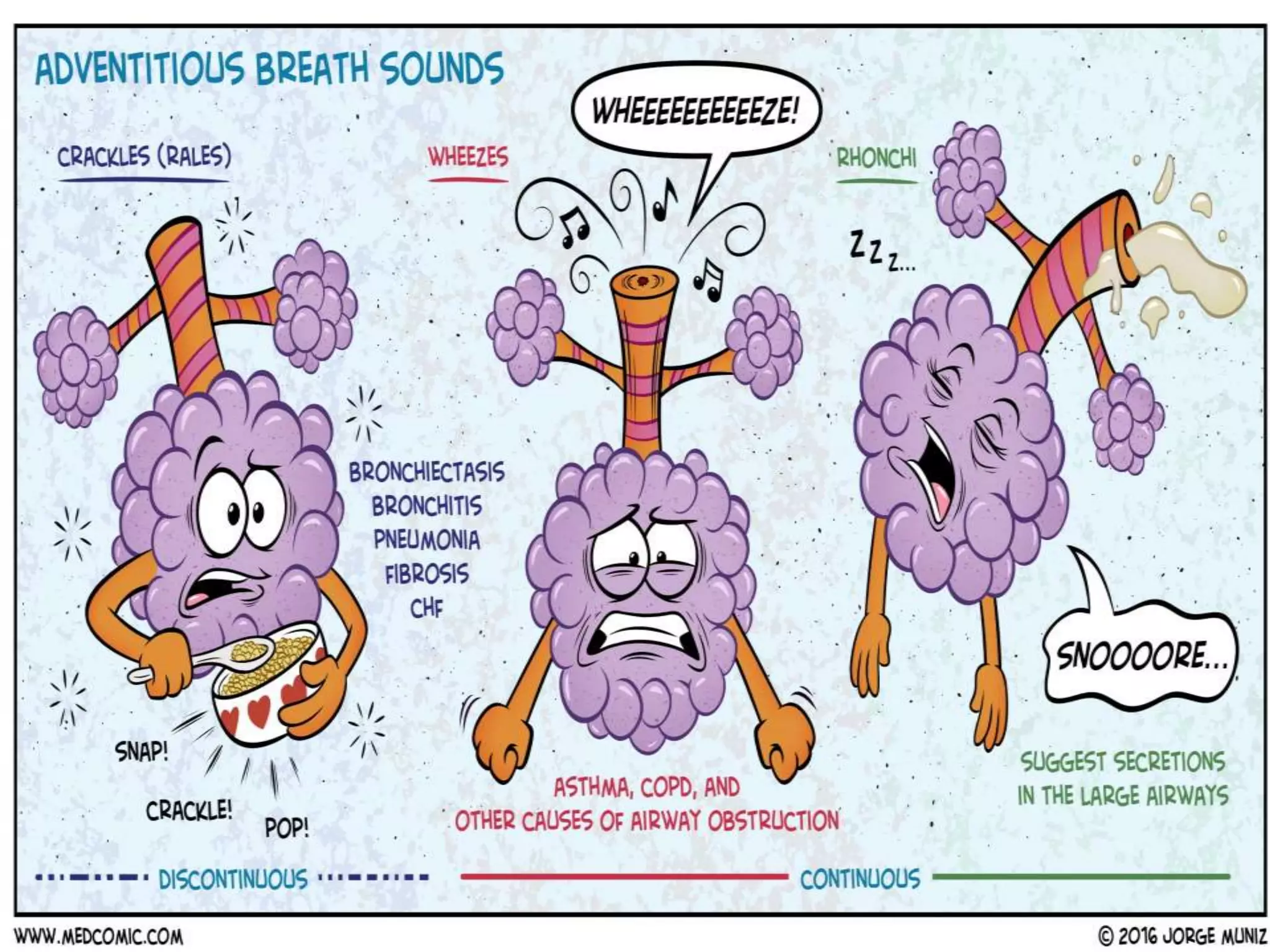
- Proper documentation of respiratory exams and scoring systems facilitates communication between providers.
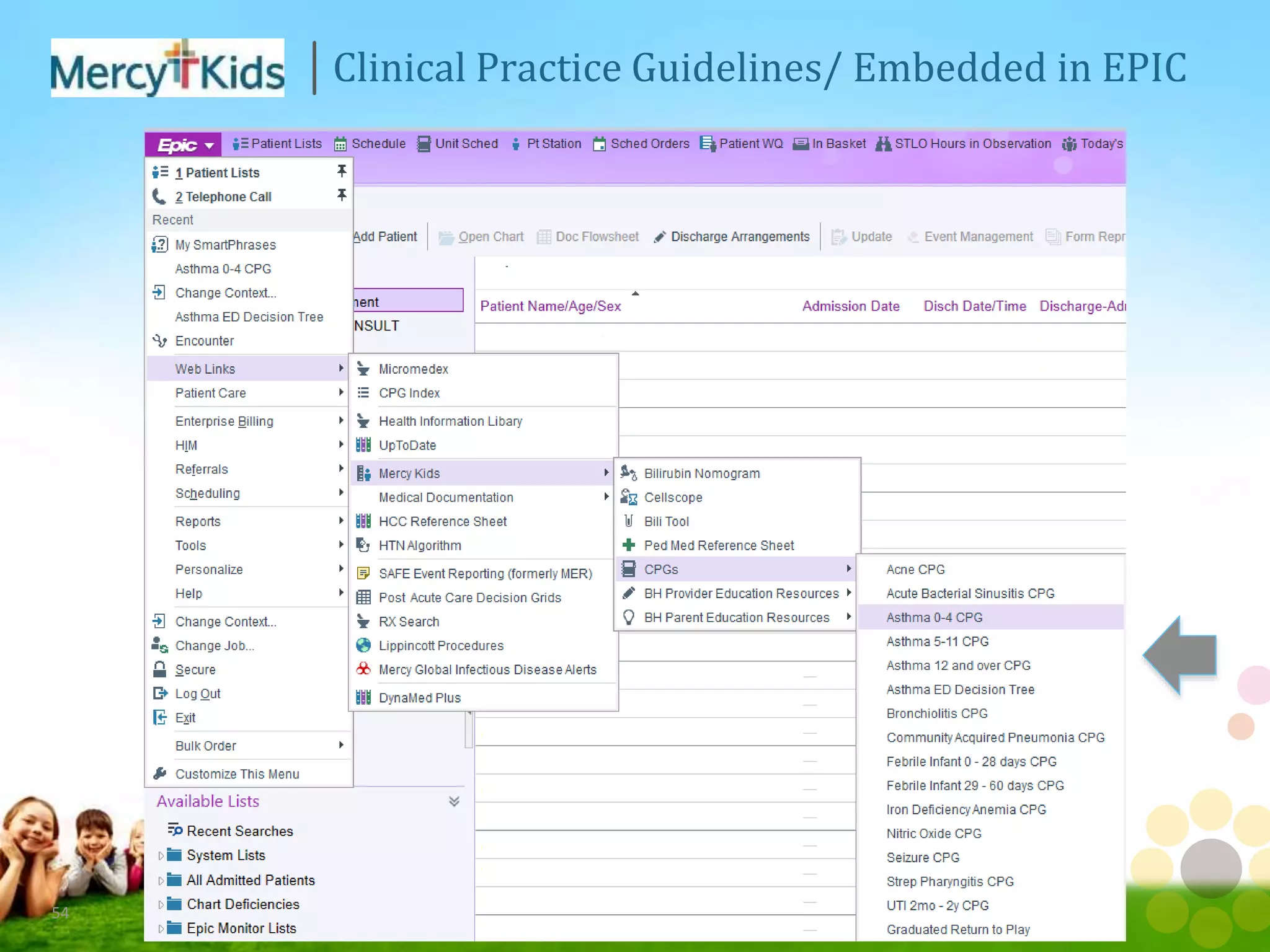
- Certification programs help standardize care and improve outcomes through multidisciplinary collaboration on guidelines, order sets, and pathways.