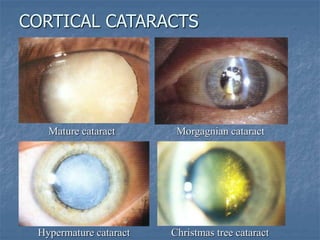
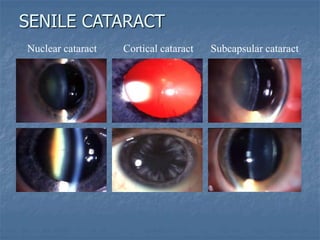
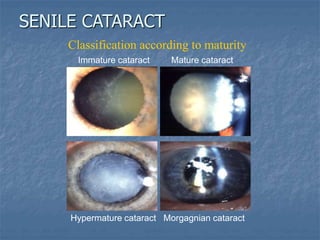
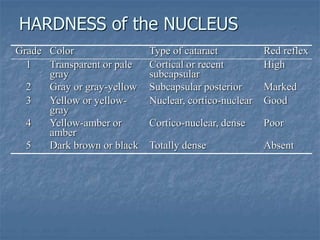
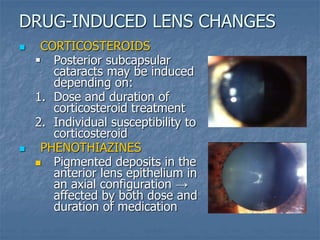
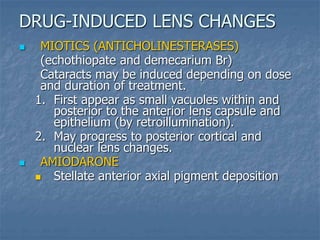
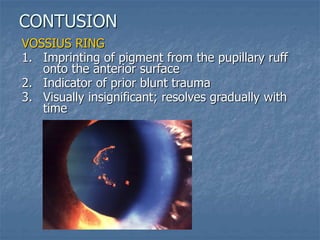
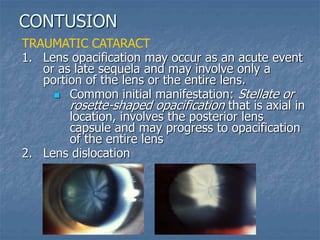
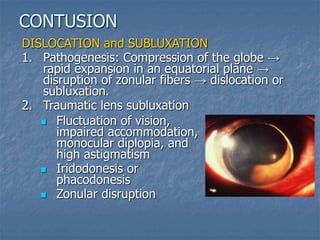
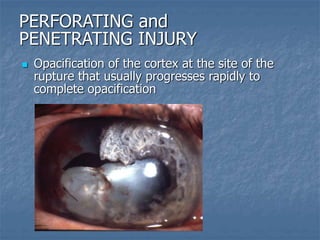
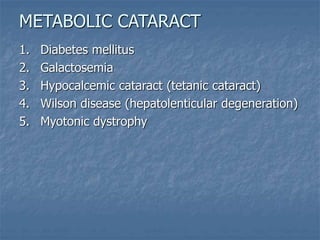
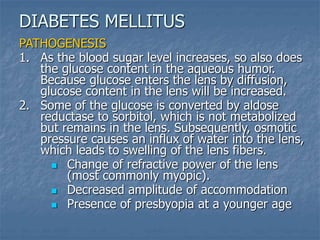
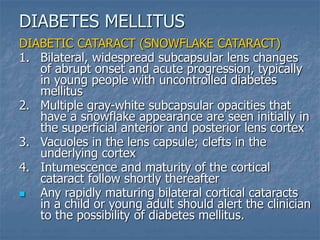
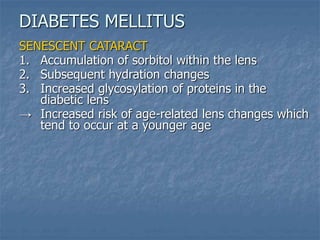
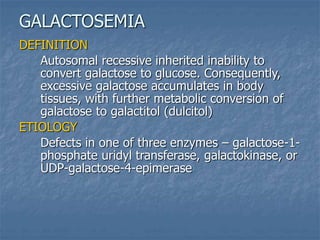
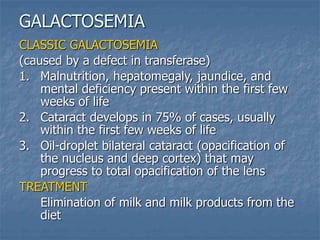
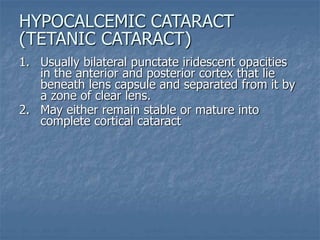
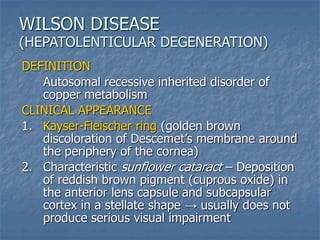
This document discusses different types of cataracts, including age-related cataracts, traumatic cataracts, and cataracts caused by other factors like radiation, chemicals, and medical conditions. It describes the typical appearance and progression of nuclear, cortical, and posterior subcapsular cataracts. Traumatic cataracts are outlined including those caused by contusion, penetrating injuries, radiation, chemicals, electricity and intraocular foreign bodies. The lens' sensitivity to ionizing radiation is also summarized.