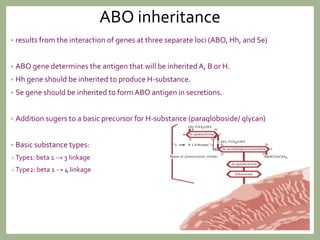
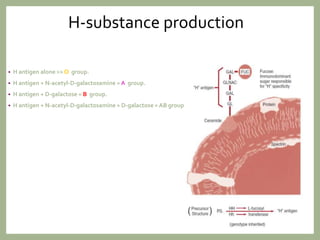
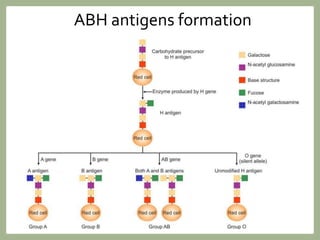
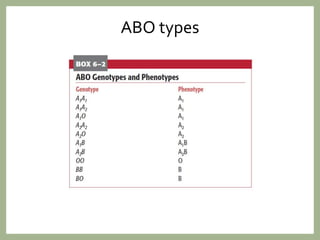
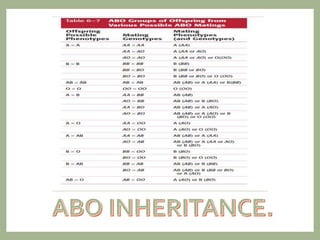
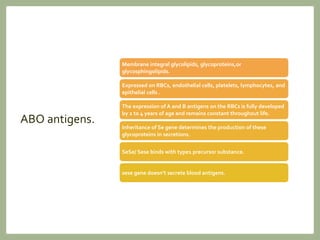
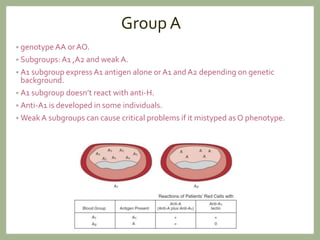
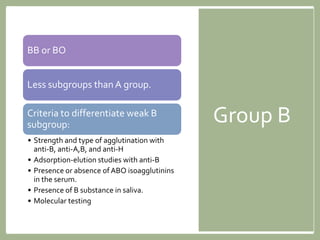
The ABO blood group system is the most important for transfusion medicine. It includes four main groups - A, B, O, and AB - determined by the presence or absence of antigens on red blood cells. ABO incompatibility between donor and recipient blood can cause hemolytic transfusion reactions. Resolving discrepancies in ABO typing results is important and may be due to technical errors, subgroups, or medical conditions affecting antibody production.