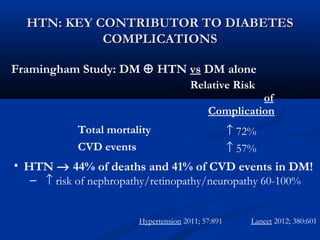
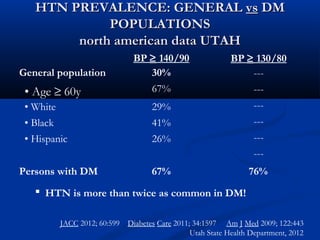
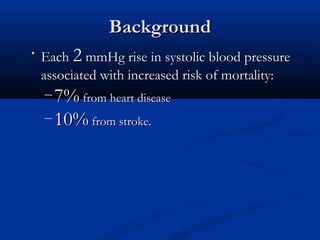
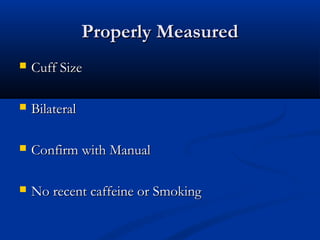
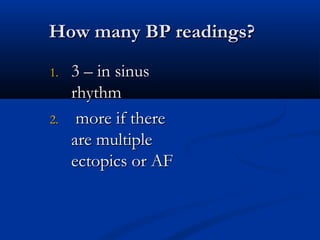
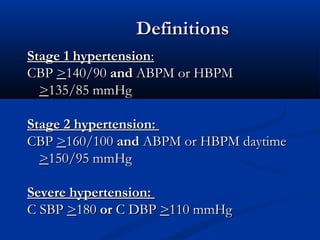
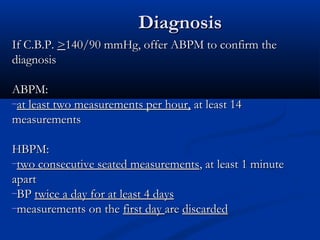
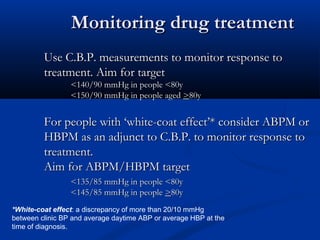
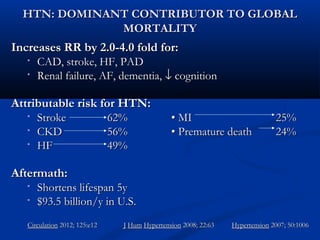
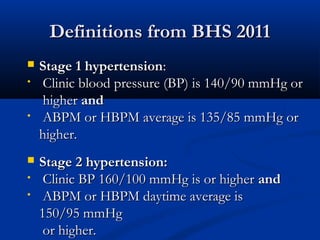
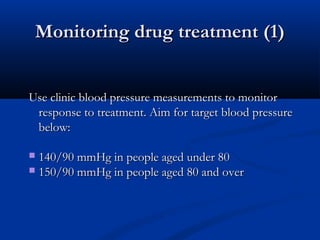
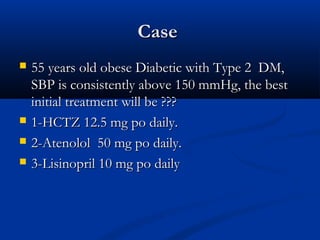
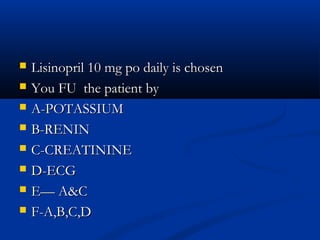
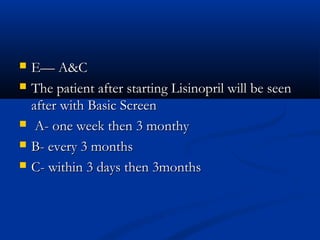
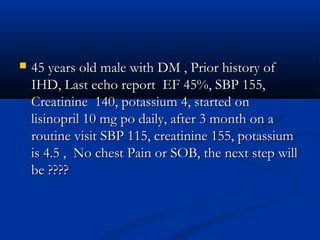
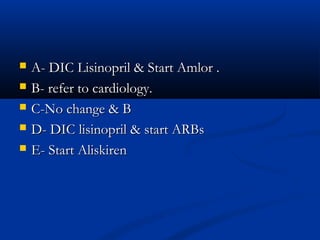
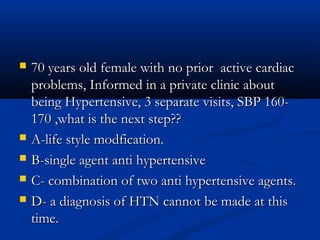
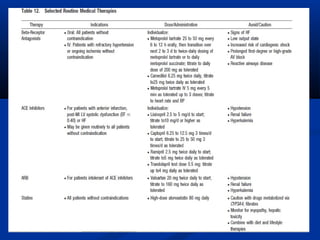
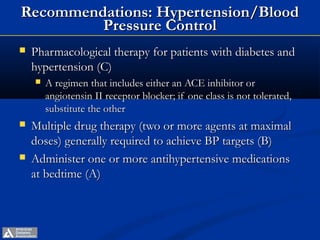
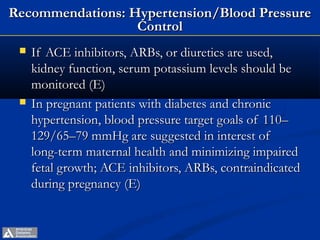
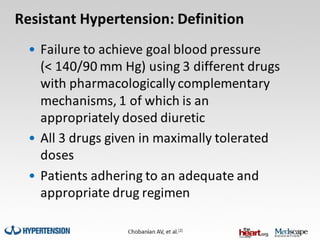
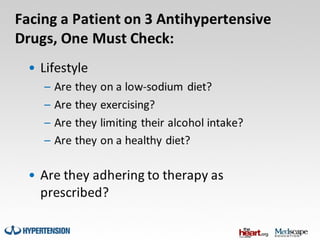
The document provides guidelines from the ADA in 2013 on hypertension and blood pressure control for patients with diabetes. It recommends screening blood pressure at every visit and confirming elevated readings on a separate day. For those over 120/80 mmHg, lifestyle changes are advised, and for those over 140/80 mmHg, pharmacological therapy should be promptly initiated to achieve targets. An ACE inhibitor or ARB is recommended as part of a multiple drug regimen, with monitoring of kidney function and potassium levels.