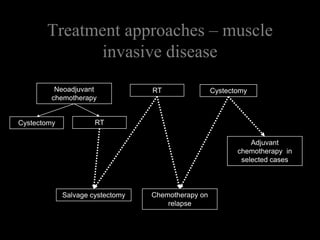
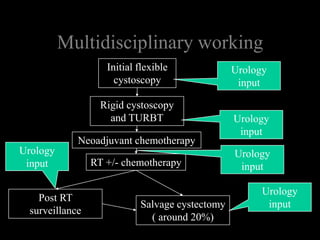
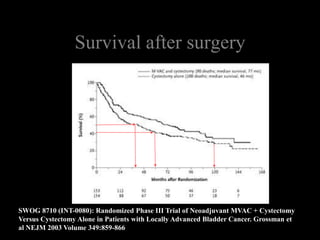
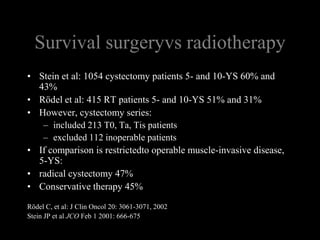
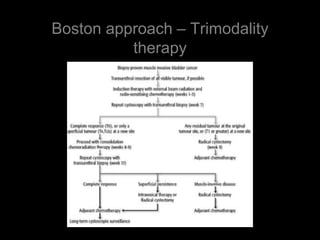
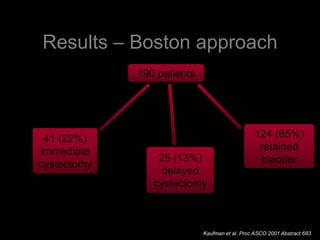
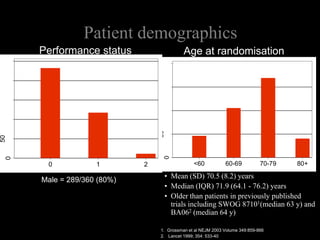
This document discusses treatment approaches for bladder cancer including radiotherapy and cystectomy. It summarizes results from several studies comparing outcomes of radiotherapy versus cystectomy, and studies combining radiotherapy with chemotherapy. The key findings are:
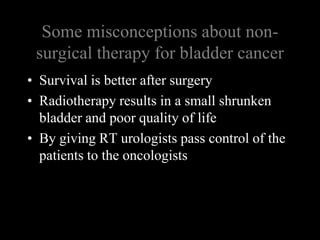
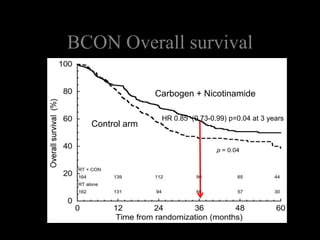
1) Long-term survival rates after radiotherapy or cystectomy are comparable.
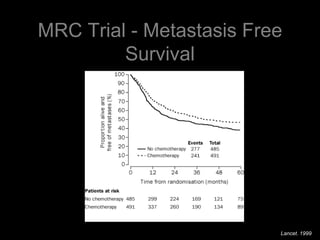
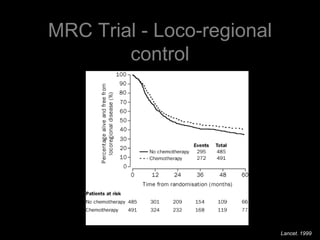
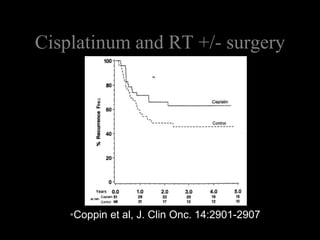
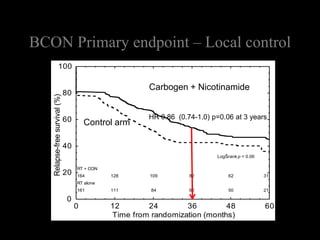
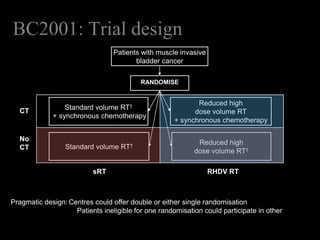
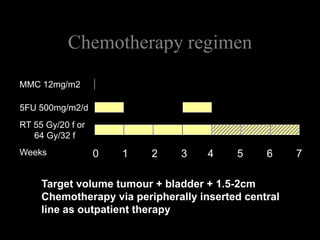
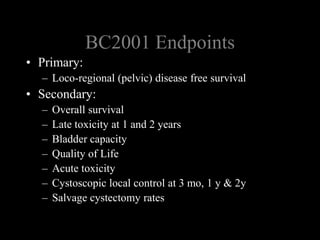
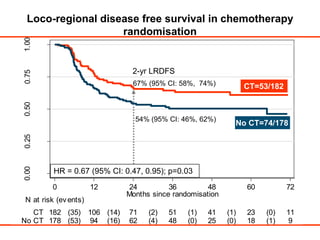
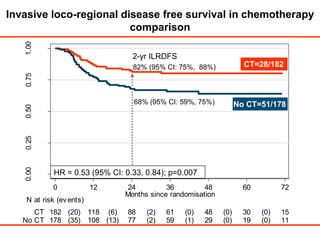
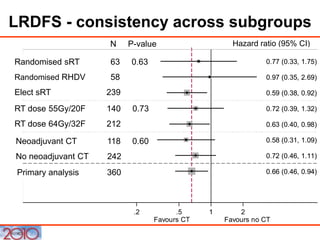
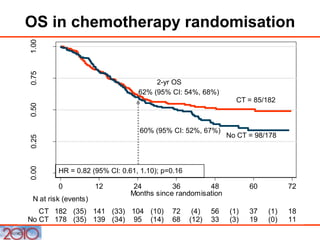
2) A study found neoadjuvant chemotherapy prior to radiotherapy improved 2-year loco-regional disease-free survival compared to radiotherapy alone.
3) Bladder preserving therapy can provide good long-term bladder function for patients who are not candidates for cystectomy.