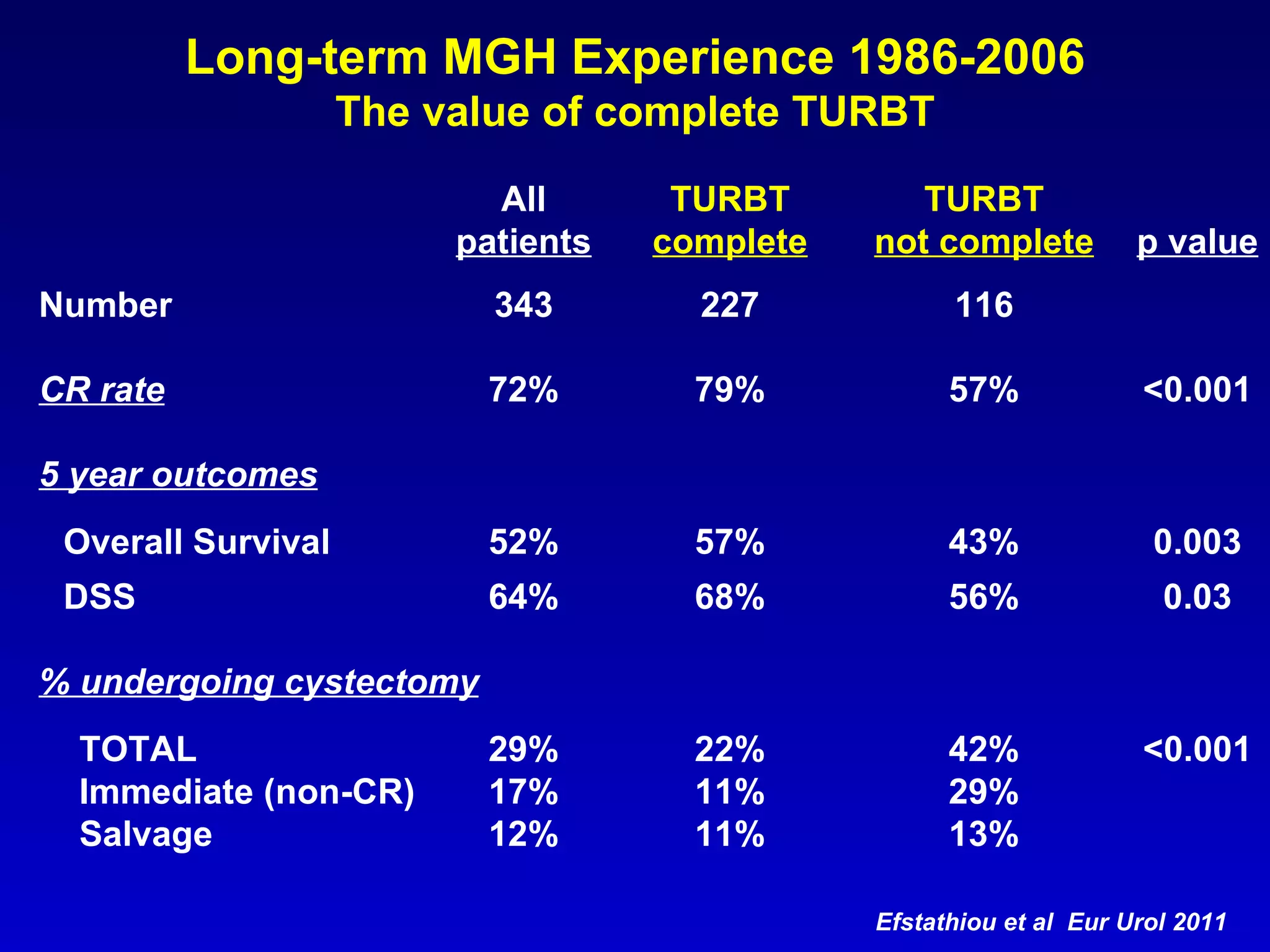
This document summarizes bladder-sparing trimodality therapy for muscle-invasive bladder cancer. It discusses the evolution of bladder-sparing approaches including maximal transurethral resection of bladder tumor (TURBT), radiation therapy, and chemotherapy. Long-term outcomes from studies at Massachusetts General Hospital show 5-year overall survival of 52% and disease-specific survival of 64% with 29% of patients requiring cystectomy. Factors associated with improved outcomes include lower clinical stage, complete TURBT, and complete response to induction therapy.