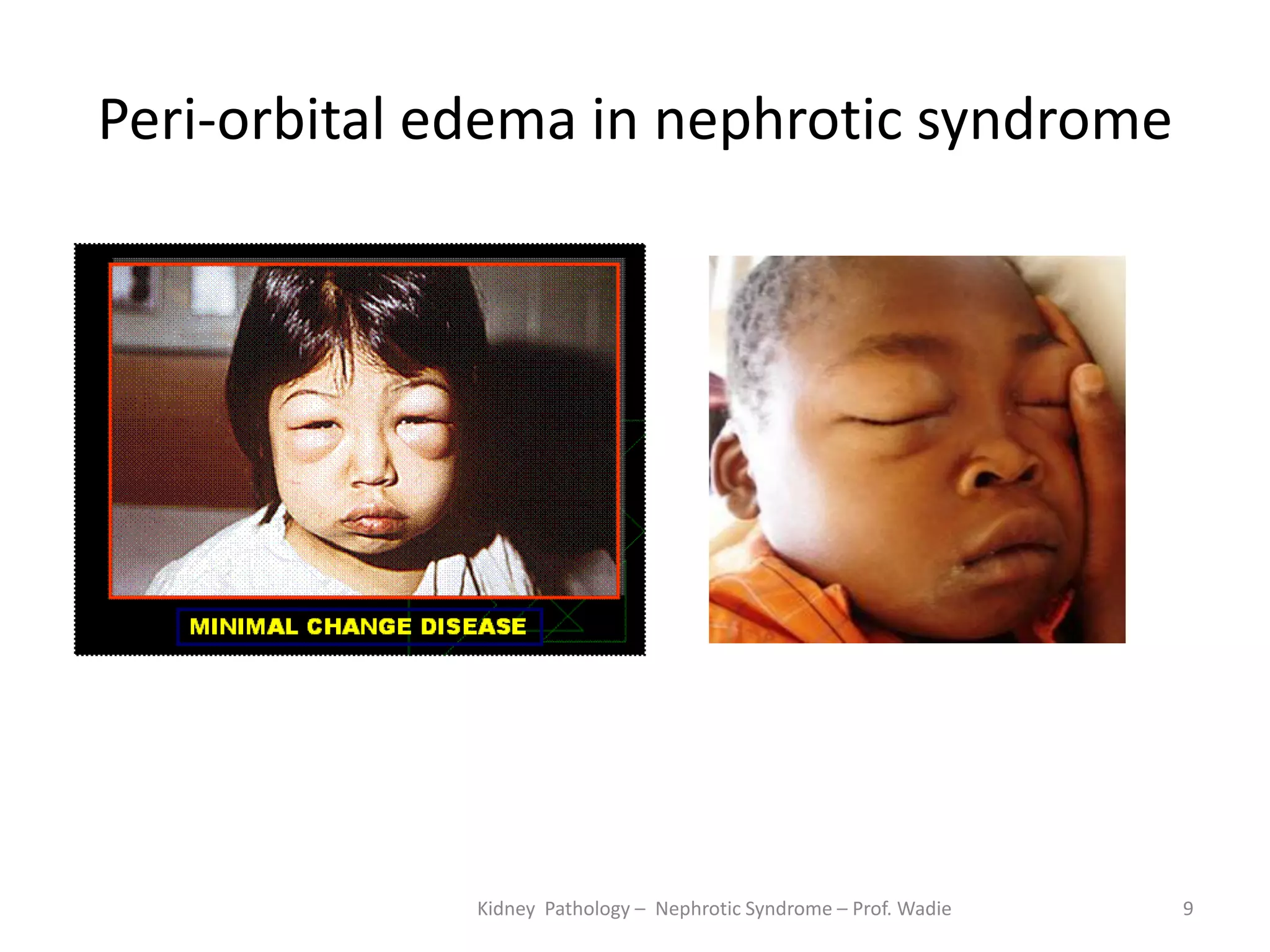
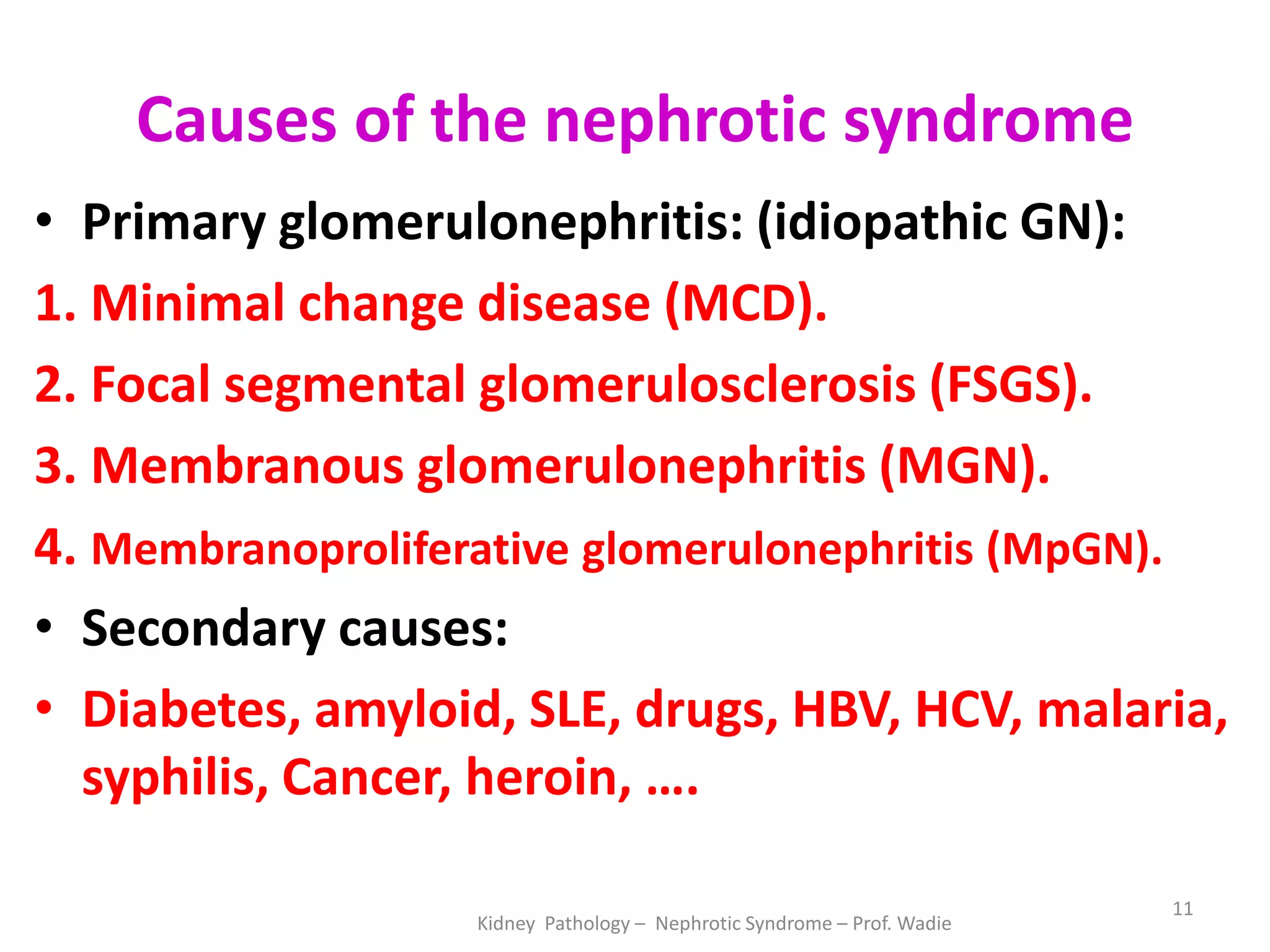
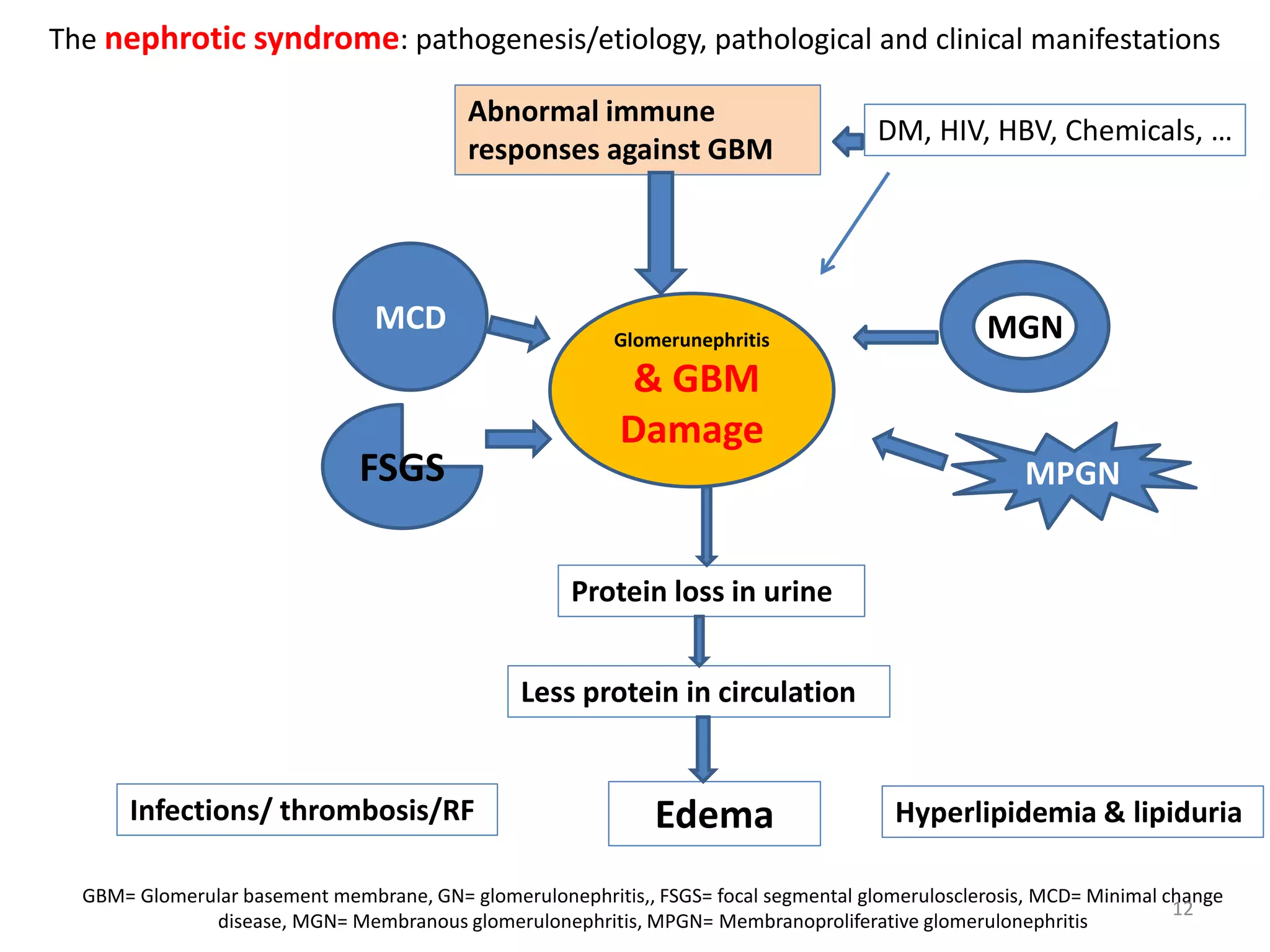
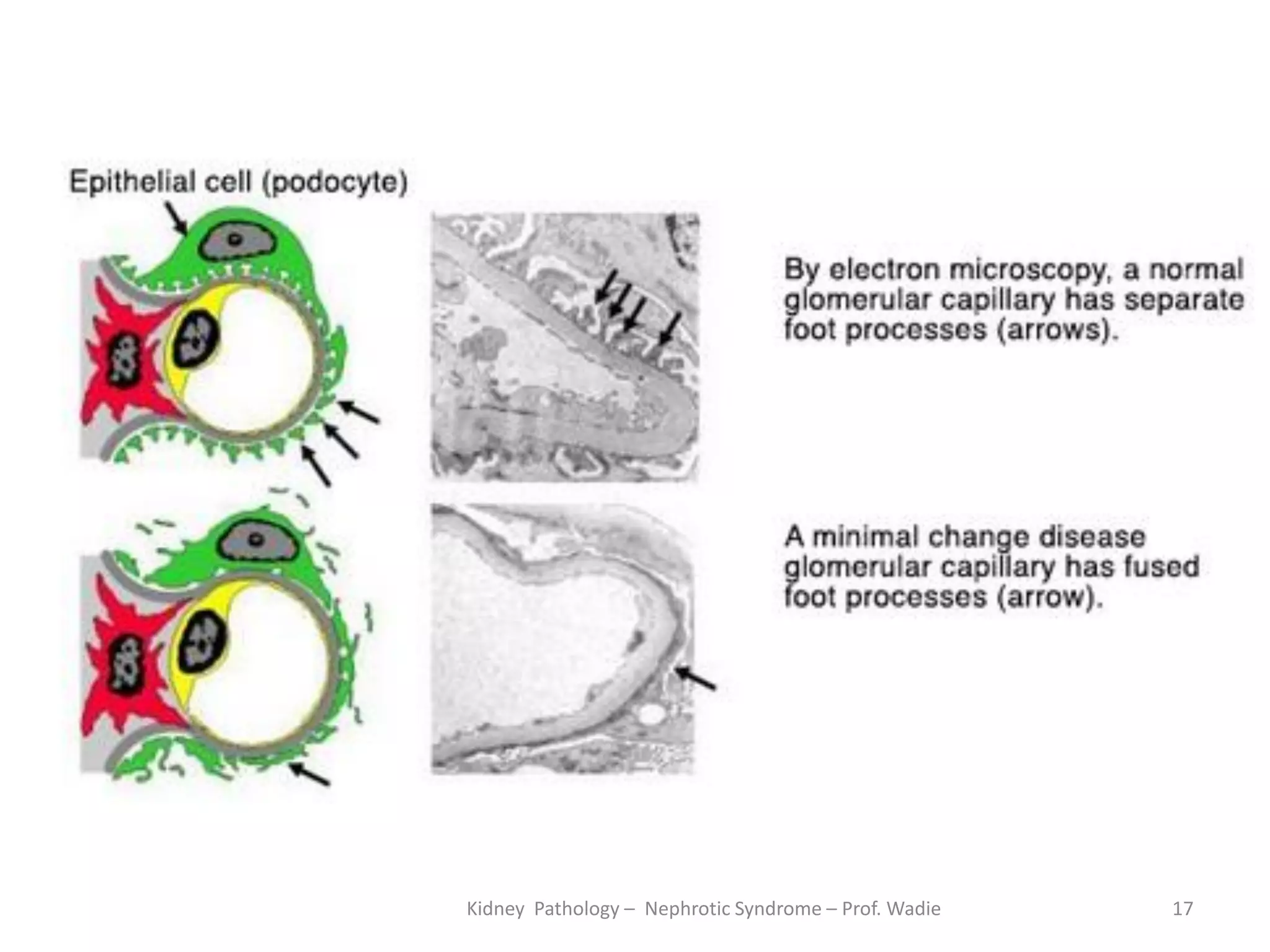
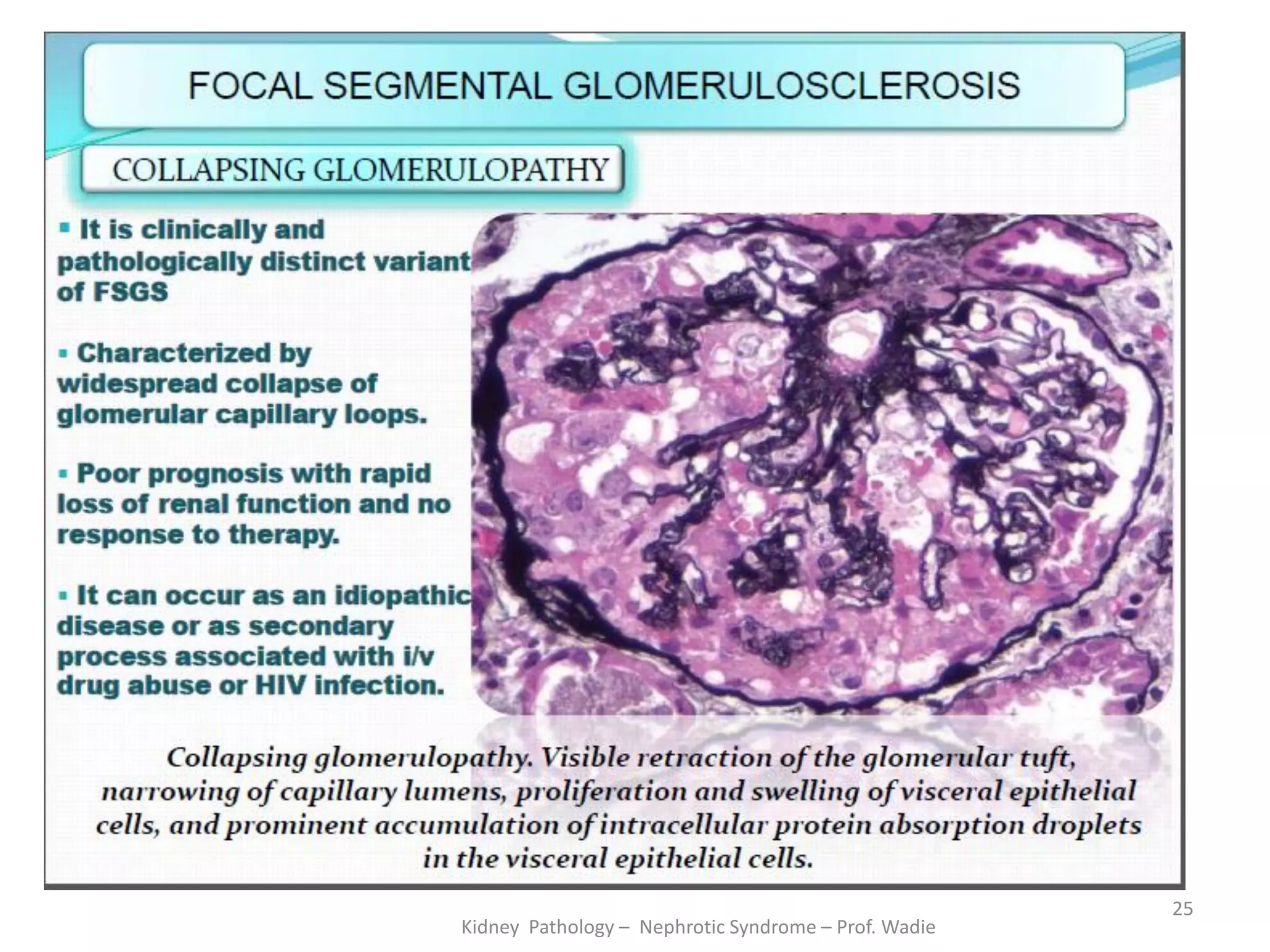
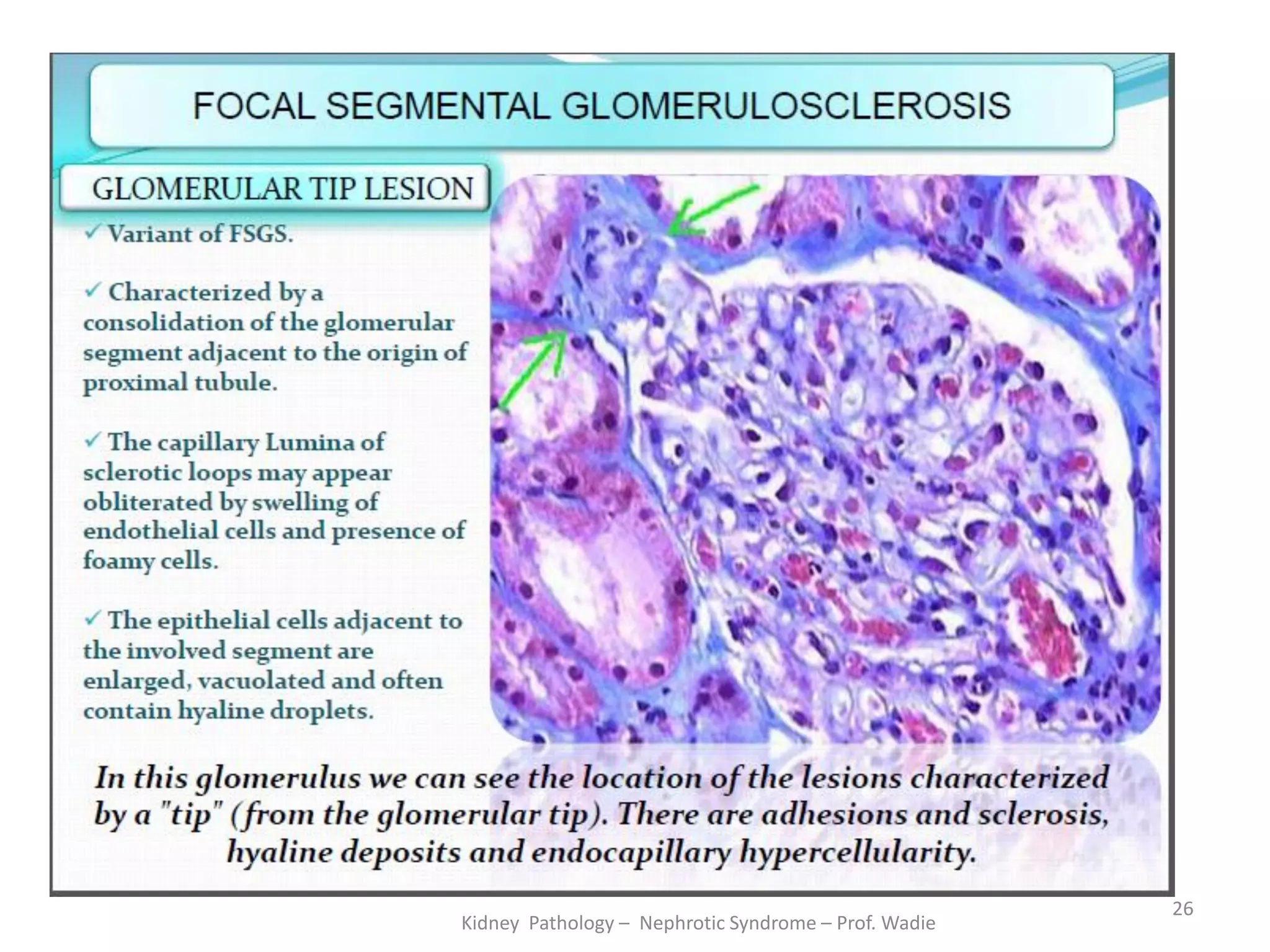
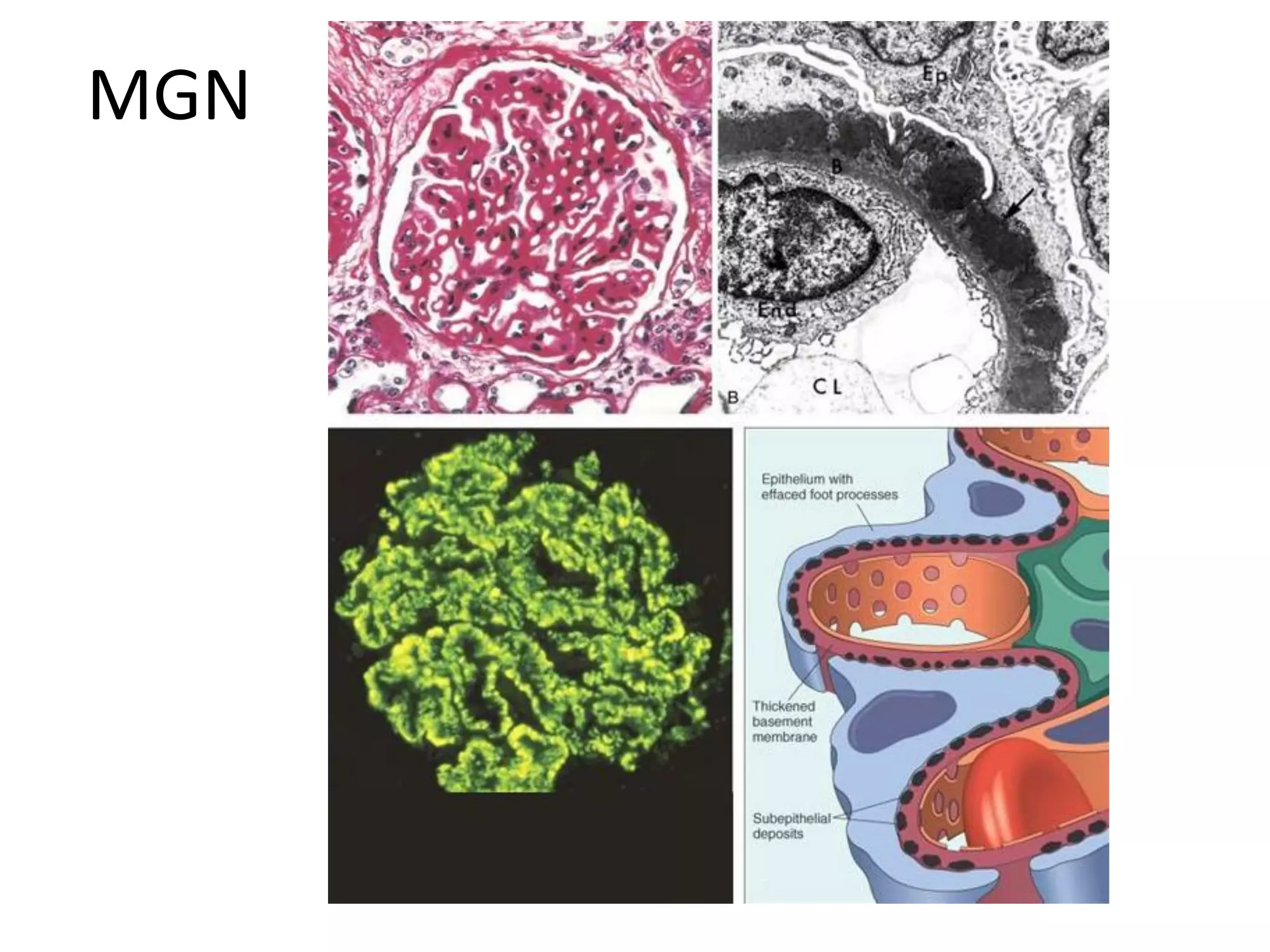
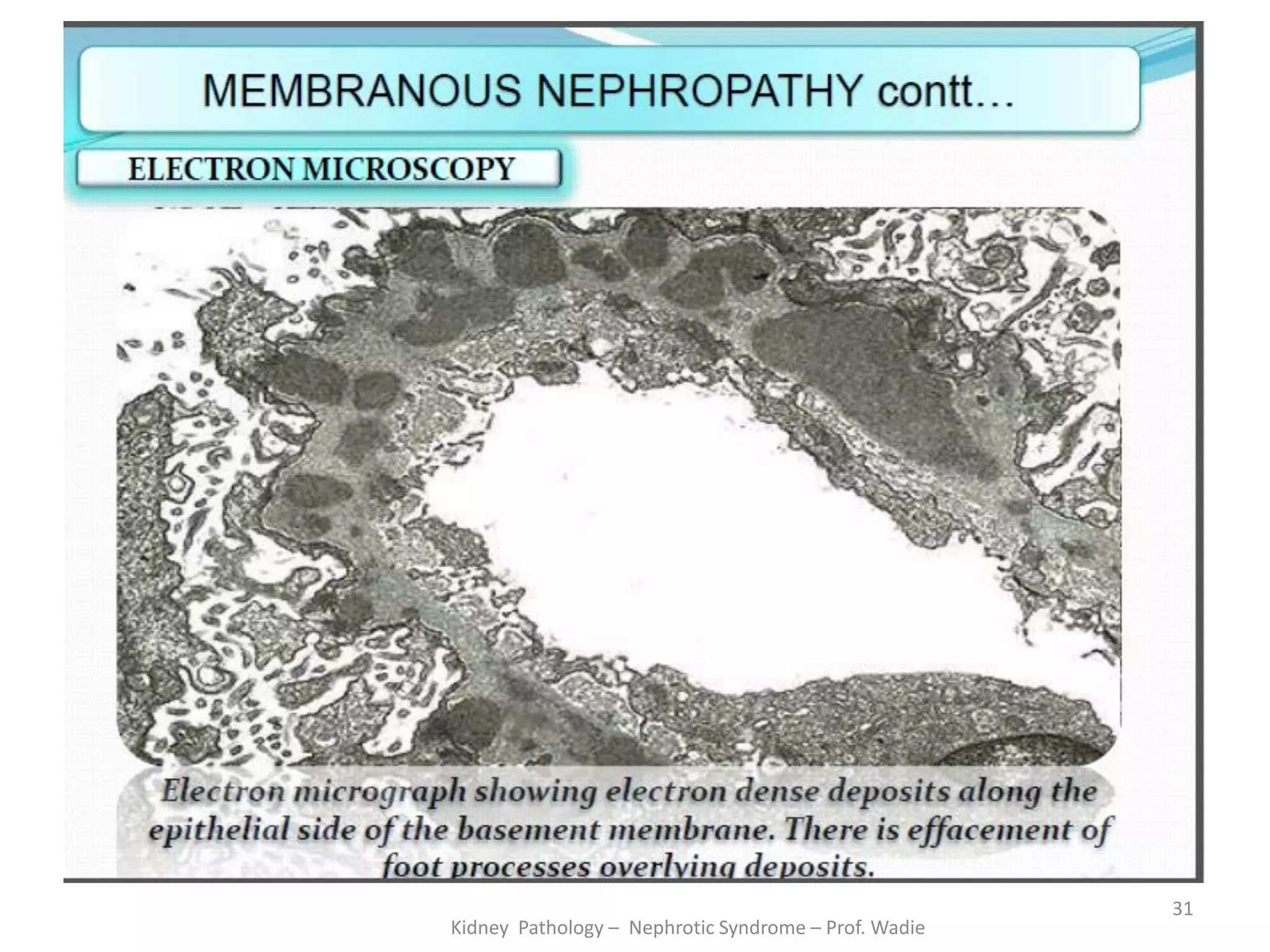
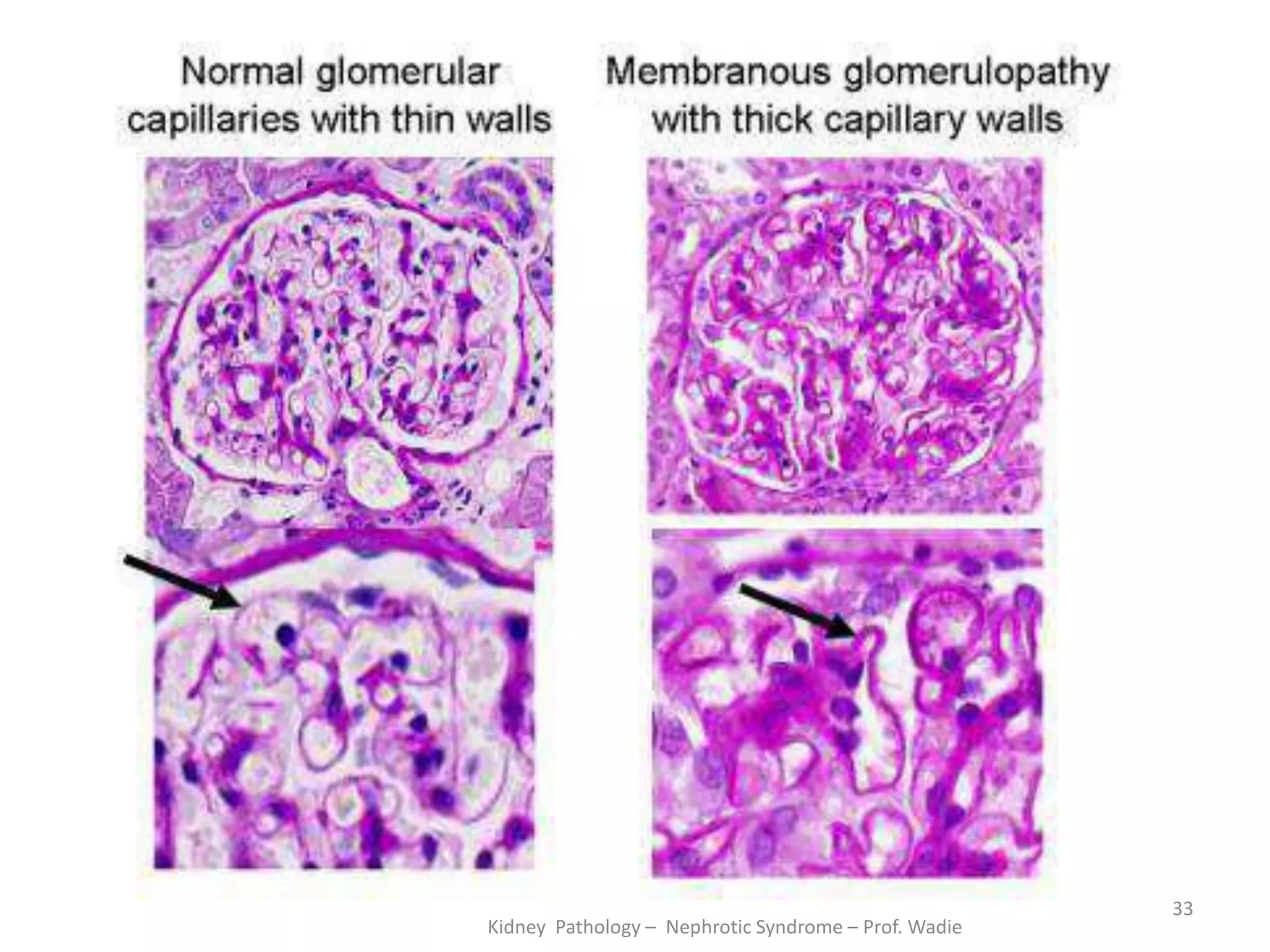
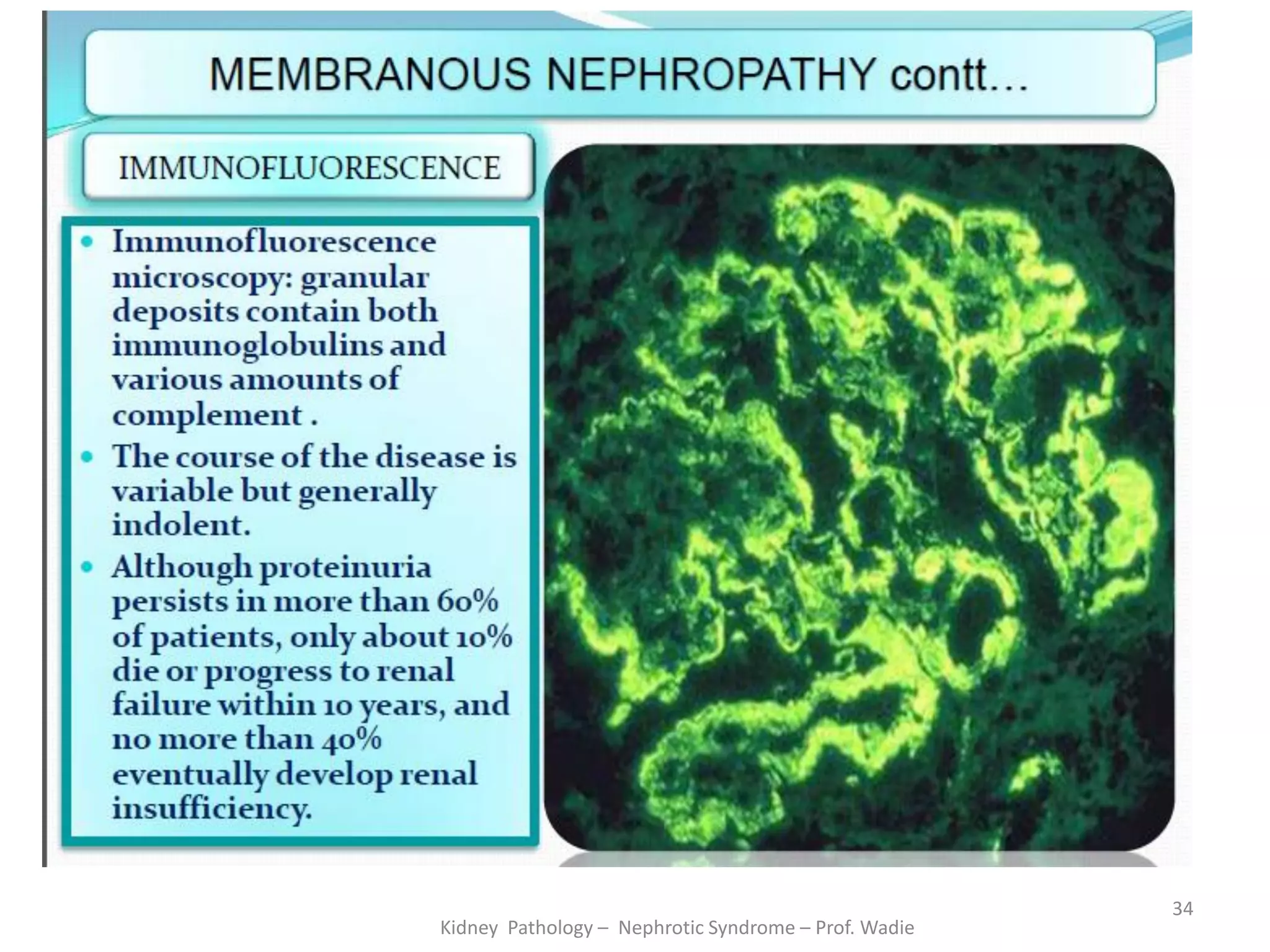
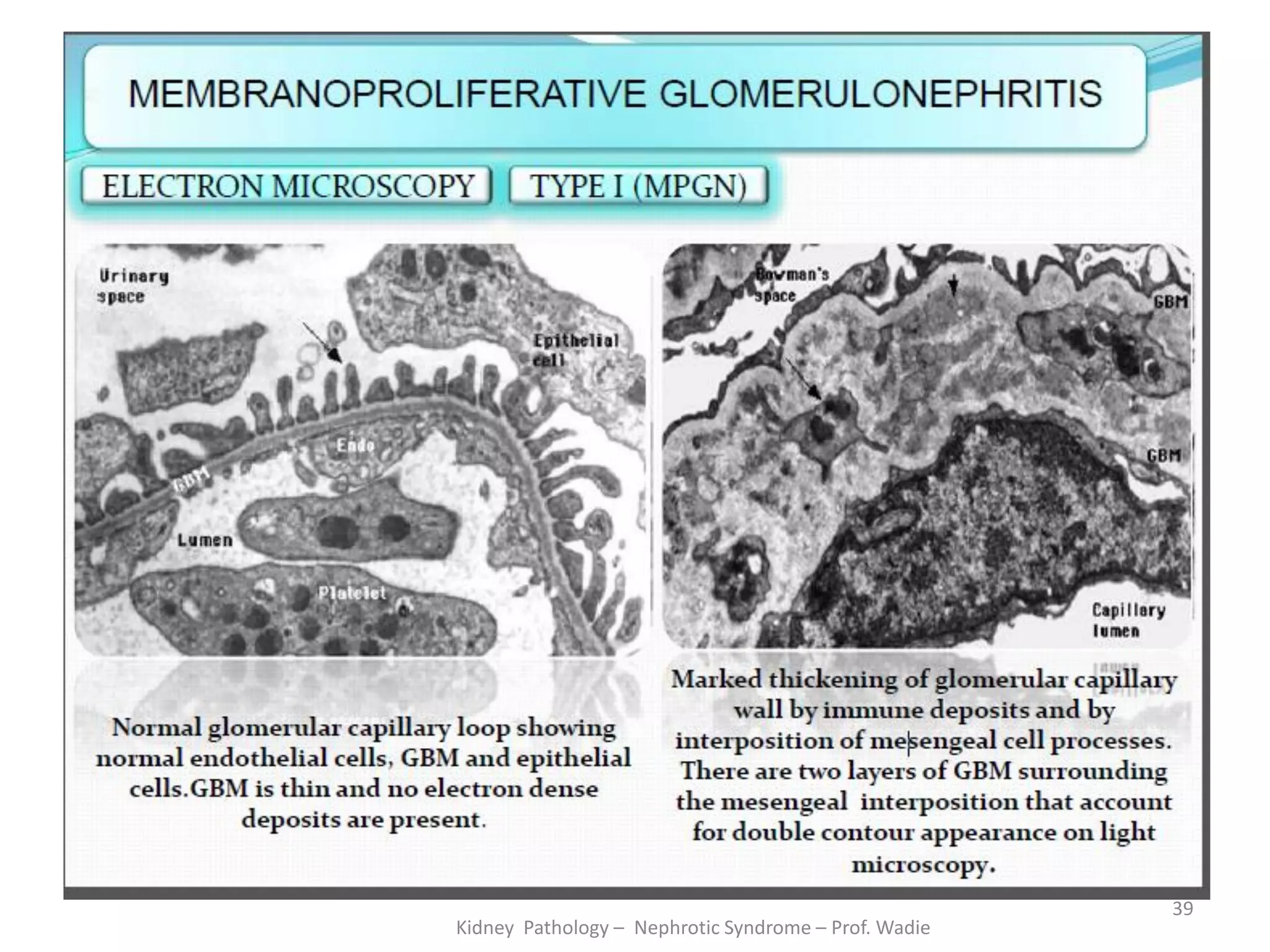
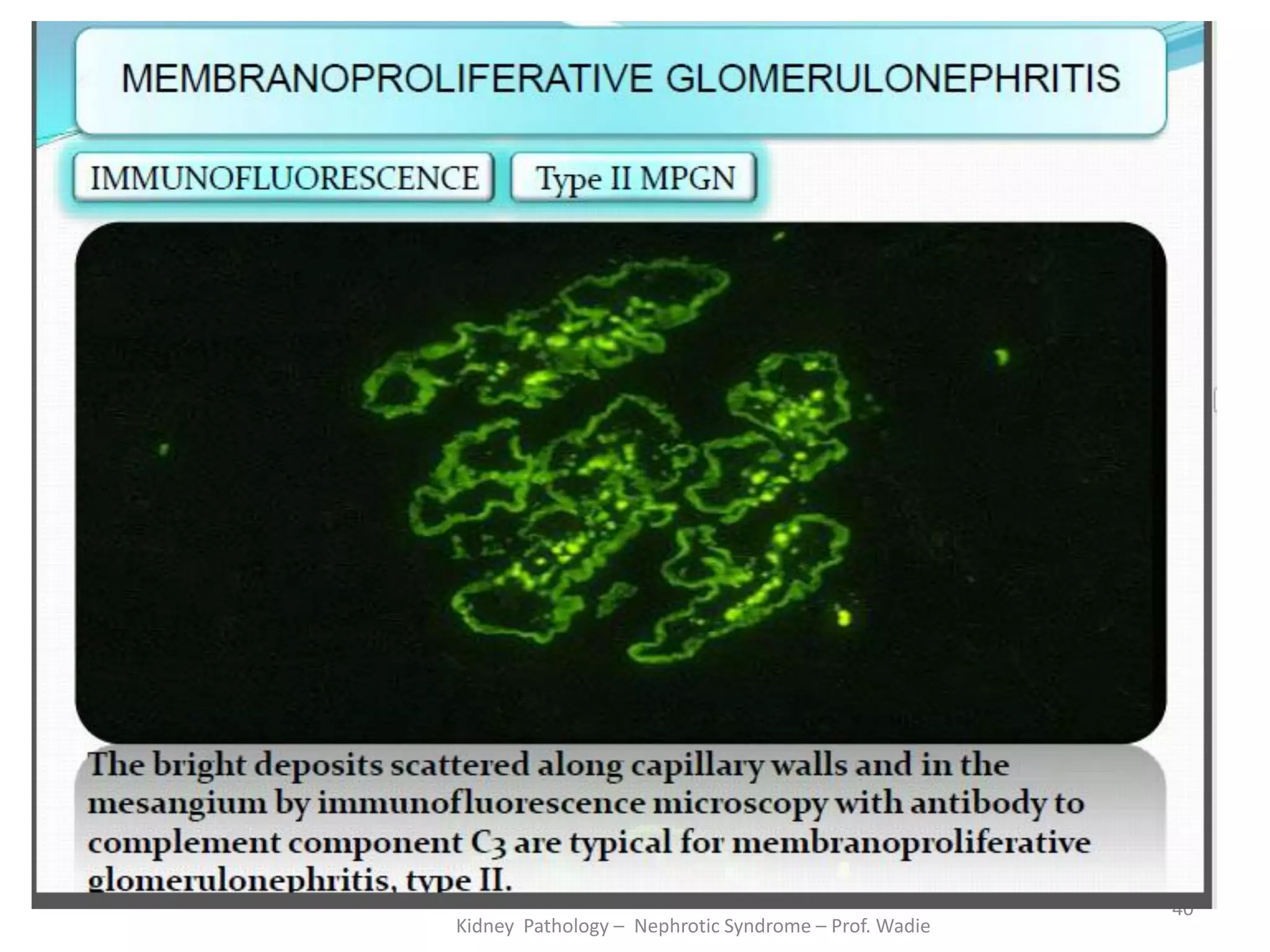
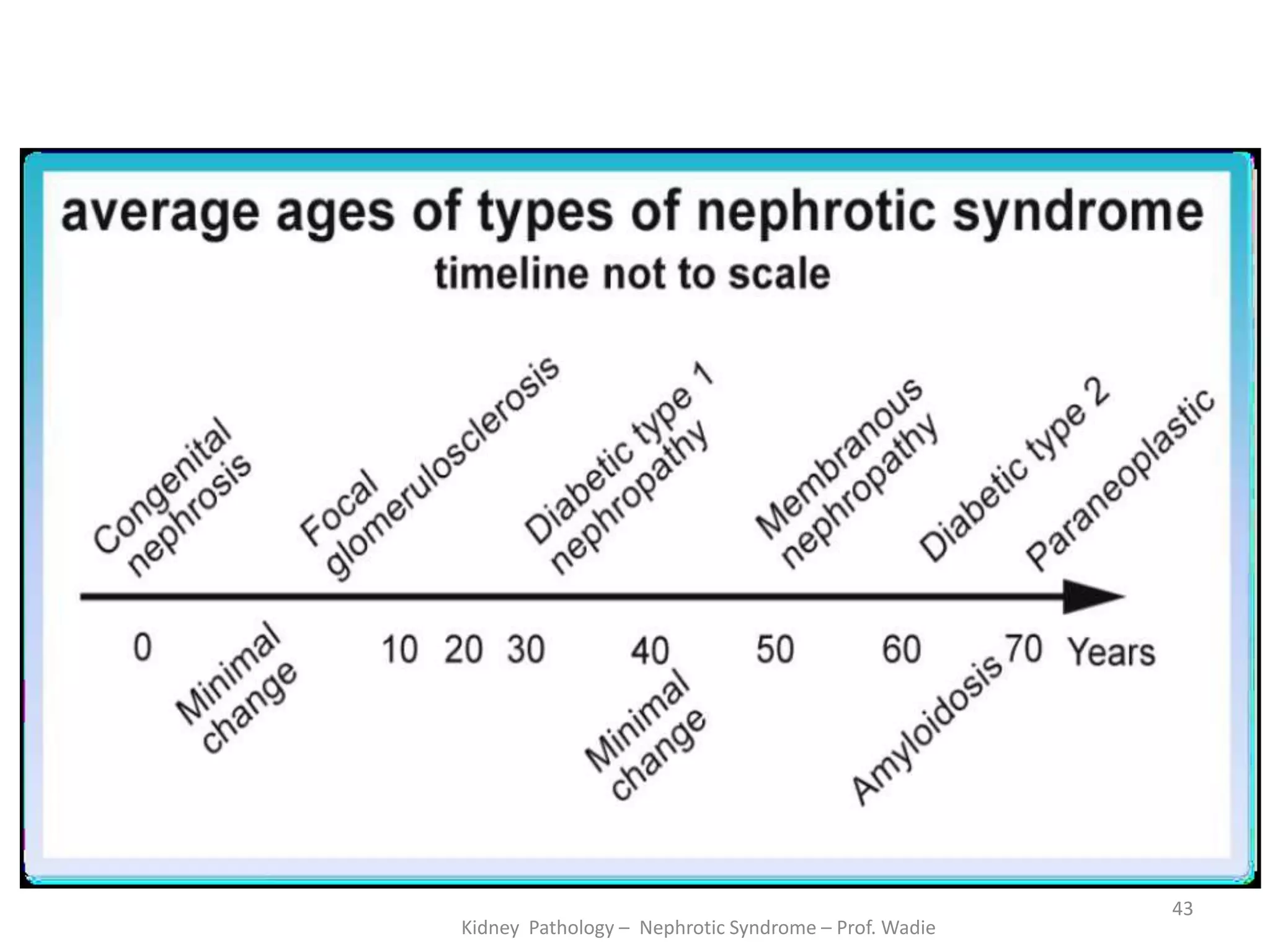
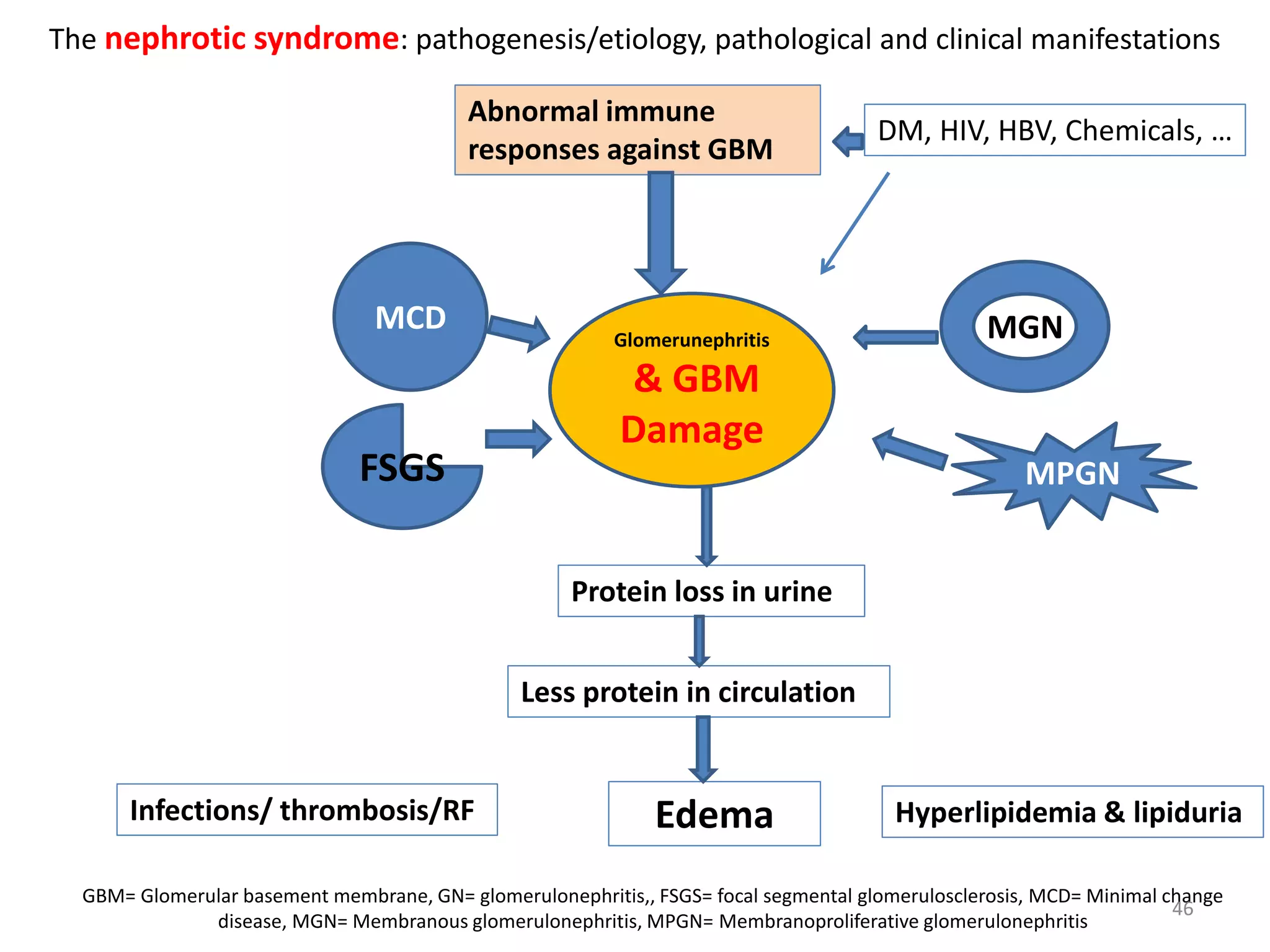
This document is a lecture on renal pathology and the nephrotic syndrome for medical students. It defines the nephrotic syndrome and discusses its main causes including minimal change disease, focal segmental glomerulosclerosis, membranous glomerulonephritis, and membranoproliferative glomerulonephritis. For each disease, it describes the morphological changes, clinical presentation, course, and pathogenesis. It also covers the complications of nephrotic syndrome. The lecture includes intended learning outcomes, definitions, illustrations, and quizzes to engage students.