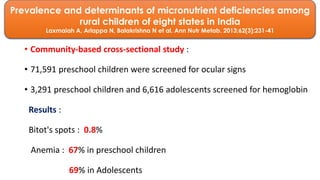
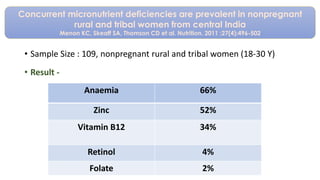
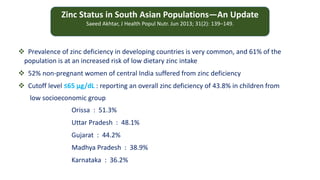
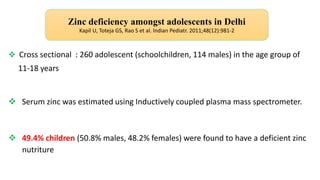
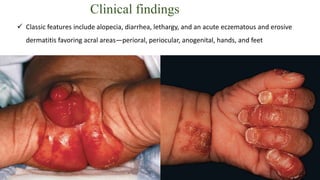
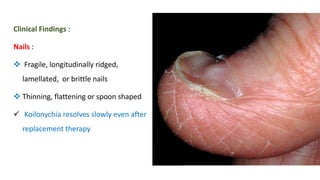
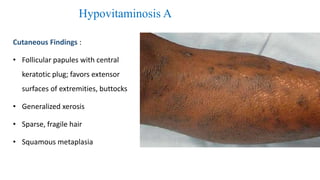
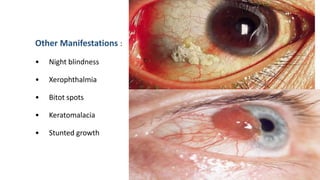
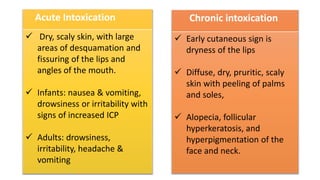
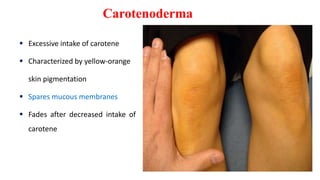
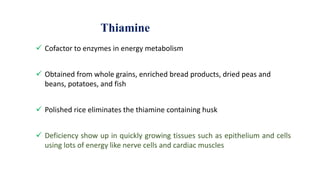
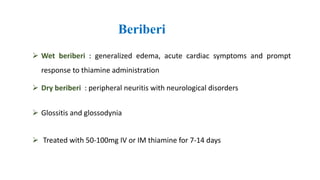
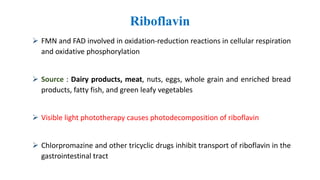
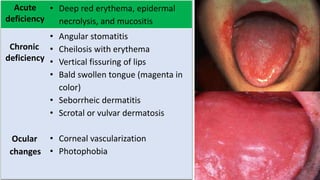
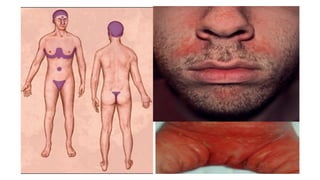
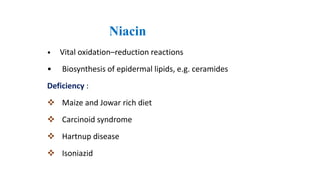
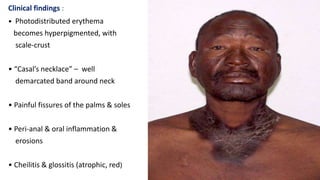
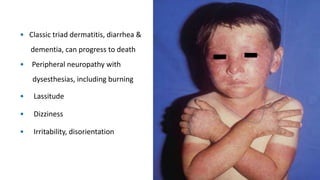
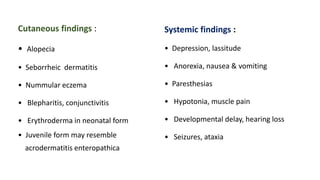
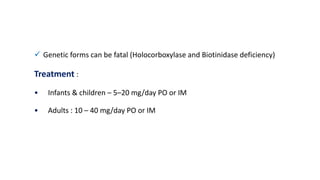
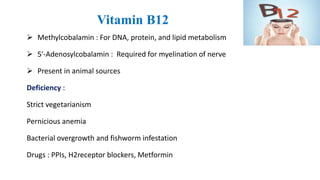
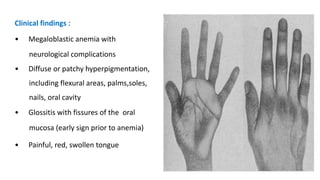
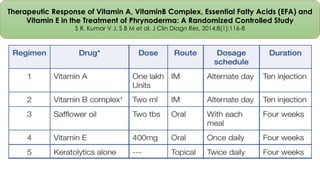
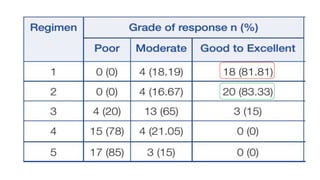
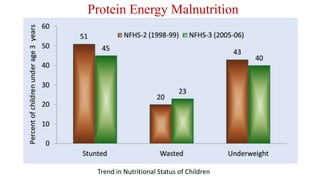
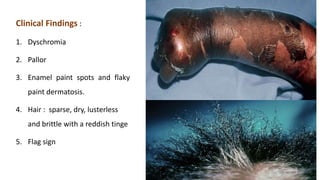
This document discusses nutritional dermatoses and deficiencies. It defines nutrients and their essential roles in the body. Common deficiencies discussed include zinc, iron, vitamins A, D, K, thiamine, riboflavin, niacin and pyridoxine. Clinical signs of deficiencies are outlined along with treatment recommendations. Studies on prevalence of deficiencies in India are summarized showing high rates of anemia, zinc and other micronutrient deficiencies.