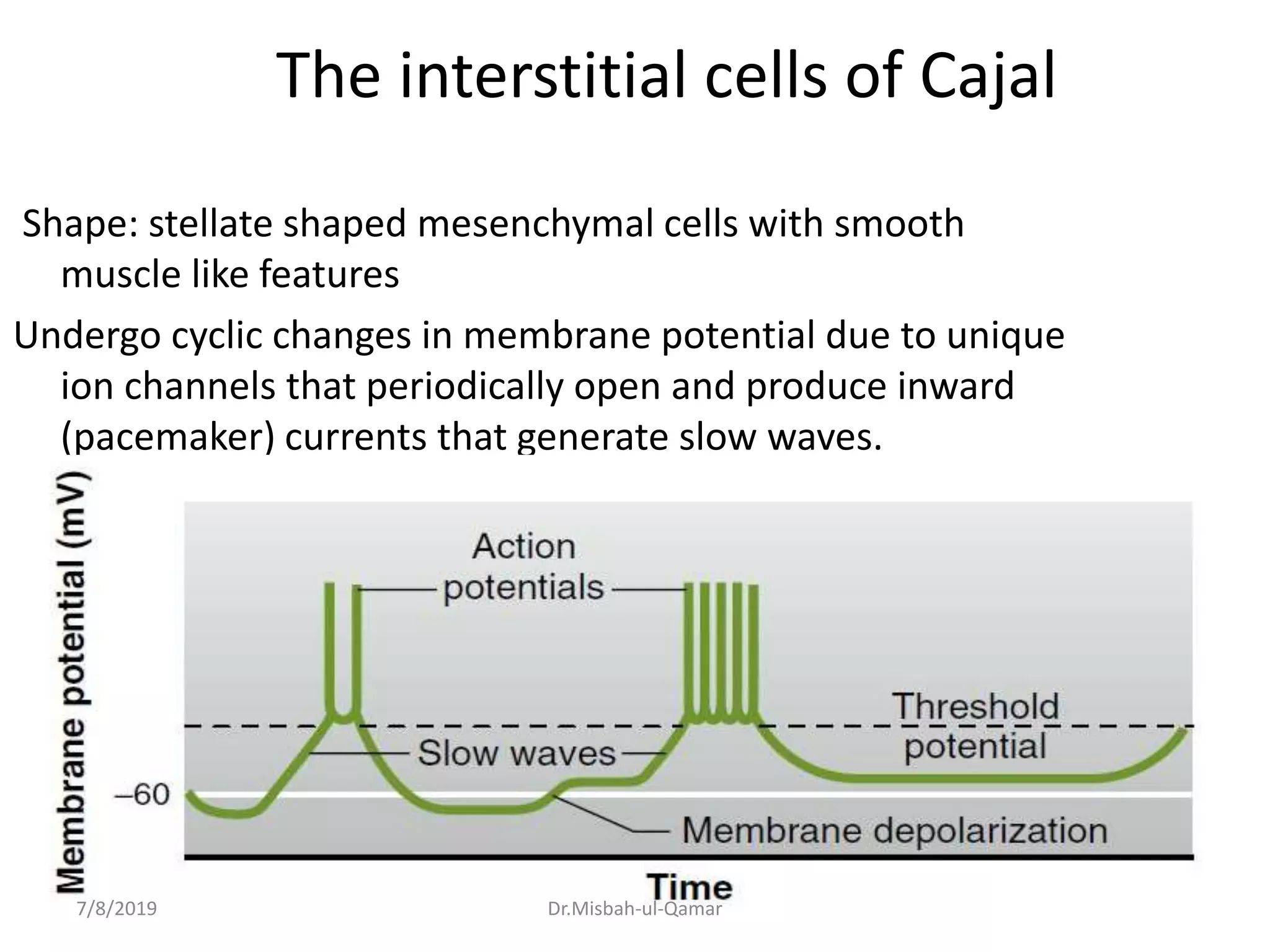
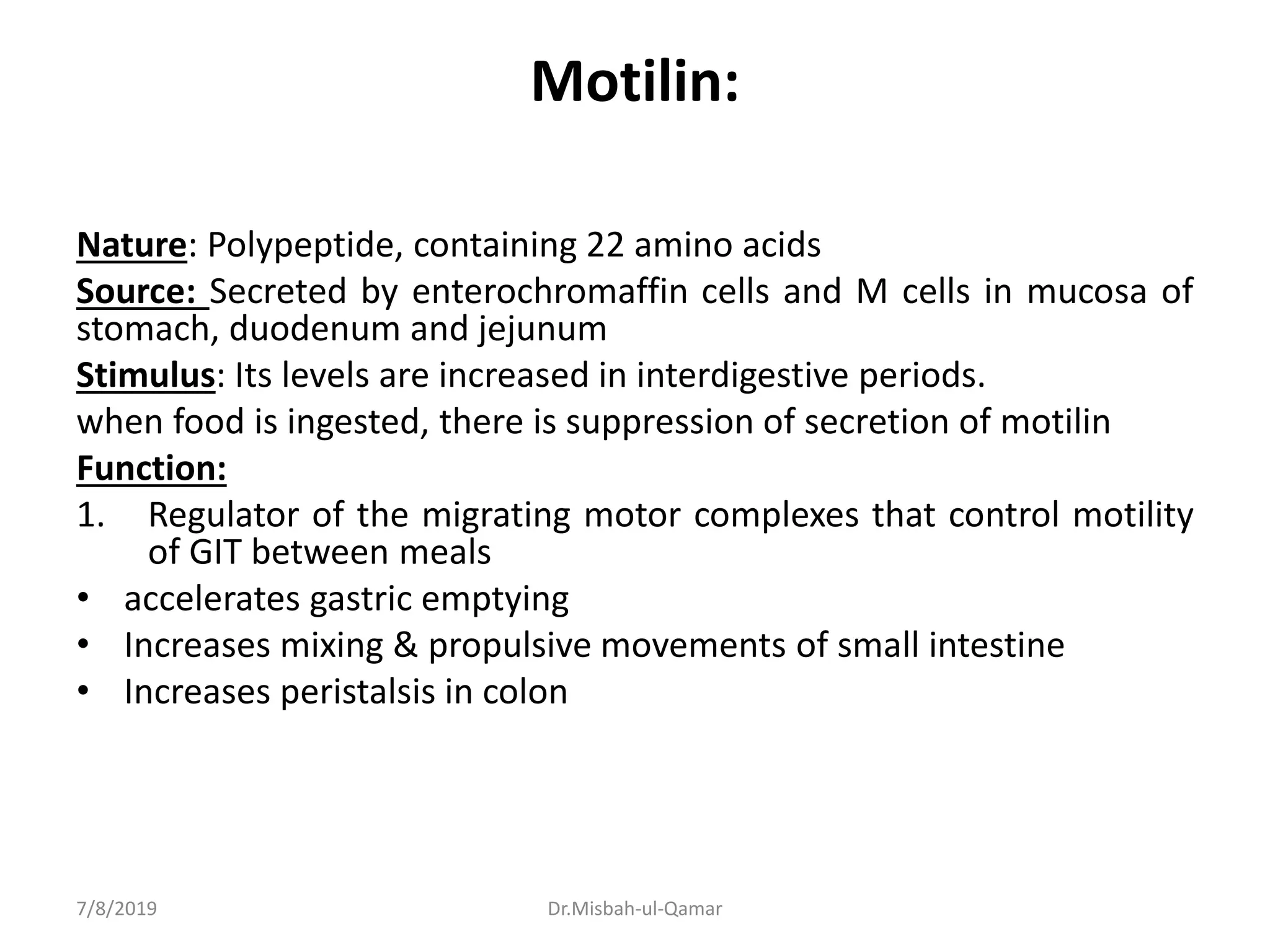
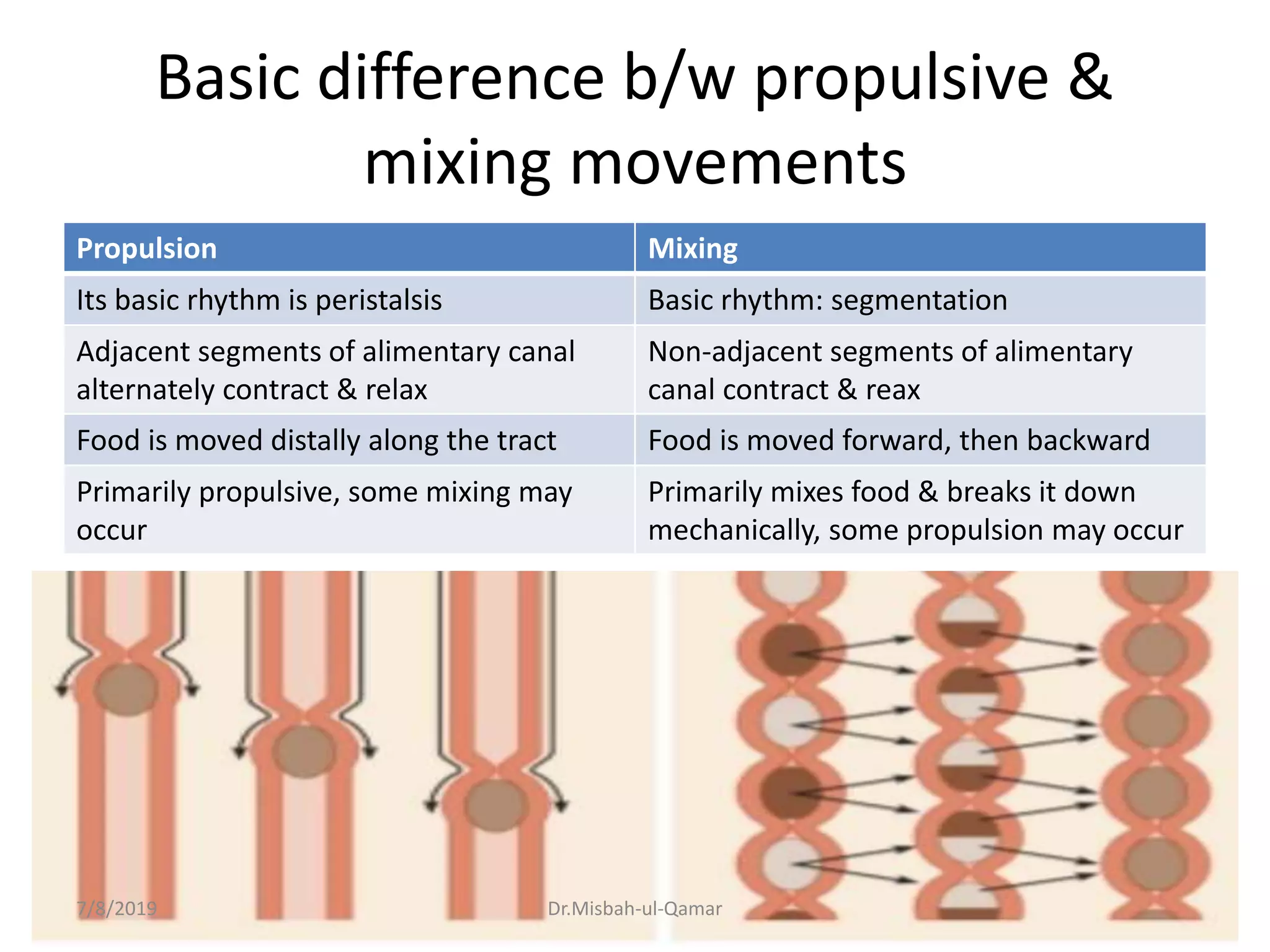
The document discusses the electrical activity of the gastrointestinal smooth muscle and its role in digestive motility. It explains that smooth muscles in the GI tract generate slow waves and spike potentials that lead to rhythmic and tonic contractions. Slow waves create the basic electrical rhythm while spike potentials cause muscle contraction. The interstitial cells of Cajal generate pacemaker potentials that coordinate peristalsis. During fasting, migrating motor complexes sweep the GI tract to prepare it for the next meal. Motility results from changes in the membrane potential mediated by excitatory and inhibitory factors.